Editorial on minimalist thoracoscopic resection of thymoma associated with myasthenia gravis
Introduction
It is imperative that the rapid development of surgical fields may benefit the patient, in particular, the healers and the medical system in general. In fact, there are undeclared achievements with the continued development of these technologies. The most important of these goals is to convince the primary supplier of patients “the neurologist” that the time has come to be more liberal in advising MG patients for surgical treatment. In the last two decades, thoracic surgery has been developing rapidly in VATS techniques. It is noteworthy that this development has begun to enter different areas, and we see the competition between new technologies so that each technique tries to prove its advantage and efficiency in providing optimal treatment for the patients, Whether by reducing the number and size of wounds “Uniportal VATS”, the use of precision technology may exceed the ability of the human’s hands “robot” or access to the chest cavity through nerveless places “Subxiphoid approach”. Over time, the number of surgeons who acquire experience and skill in minimally invasive techniques will increase. In the near future, thymectomy for MG patients via sternotomy or thoracotomy will be only part of the history. In this article, we review the stages of the evolution of the approach to thymectomies from the beginning to the present with regard to the article Pompeo and his colleagues (1) and our perception of the future of less invasive thymectomy.
Discussion
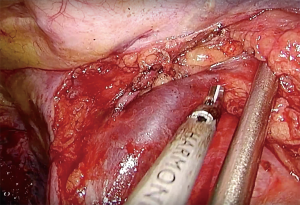
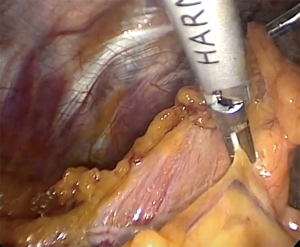
More than 75 years have passed since the scientists began to resect the thymus gland in order to treat or decrease the symptoms of Myasthenia Graves believing that the thymus to be the key to the pathogenesis of MG as a source of antibodies directed against acetylcholine receptors (2). Since then, surgeons have begun to develop surgical techniques to avoid sternotomy or thoracotomy because of the side effects and complications that may accompany these techniques. The beginning was from the full mid-sternotomy approach which remained the gold standard approach for a long period (3). Later, there were attempts to make it less invasive through the development of partial sternotomy (4). Then there were efforts to enter the mediastinal cavity through the neck without the need to incise any part of the sternum (5). However, because of some disadvantages such as limited exposure, incomplete excision of the thymus, and difficulty controlling some of the complications during the surgery such as bleeding, these techniques could not replace the sternotomy (4,5). With the development of endoscopic camera technology and the start of the utilization of thoracoscopic operations, minimally invasive techniques began to appear in the scene as techniques that support in traditional surgeries before starting to take the banner of lead and be the main agent in the procedure (6-9). Since the advent of thoracoscopic techniques as an alternative to conventional surgery, there has been near consensus that it is better for the patient and the surgeon. But debate and controversy is still on the approach (10-16). There have been many standpoints about the ideal place to enter the thoracic cavity, from the right side, left or both sides at the same time. It seems that access from the right side is the preferred technique for most surgeons because it provides excellent exposure for the Innominate-Caval junction (ICJ) (Figure 1), in addition to the presence of the heart in the left side, which may impede the instrumentation. Pompeo relies routinely on right side access in his technique side and many colleagues may agree on this. On the other hand, there are some surgeons who prefer to enter from the left side, and those believe that this access may provide better vision for the pericardial-phrenic and A-P window regions, these areas are considered to be one of the most common areas of ectopic thymic tissue (15) (Figure 2). There are those who believe that VATS thymectomy procedure should be performed bilaterally for the best results. However, these results were not proven as there was no difference in the rate of remission and the sample weight was not different between the unilateral or bilateral technique (16). Reducing the number of the surgical incisions and developing the VATS technique uniportal VATS approach for thymectomy has reduced surgical trauma, improved cosmetic appearance and reduced surgical pain, but has not resolved the dilemma of the approach (17,18). Is it better to enter the thorax from the right, left or both sides?
Parallel to the evolution of VATS, the robot (RATS) began to appear as a strong competitor and carried with it good results in terms of remission that may exceed the results of the VATS in addition to its surgical Endo wrist demonstrates and rotates 360 degrees with seven degrees of freedom, and the movement of the range with the vibration filtration system makes more precise maneuvers (19). However, the robot is still not available in most of the centers and its high cost is a considerable obstacle to the progress of the RATS in addition to the fact that the robotic surgery is still multi-portal. With the beginning of the new millennium, another motivating technique began to emerge, approaching the anterior mediastinal space from below the sternum (subxiphoid approach). Initially, this technique was complementary to intercostal VATS technology or transcervical technique (20,21). As time passed and surgeons gained experience and skills, this technique began to evolve until it became applied through the single port (22,23). There is no doubt that the subxiphoid approach has many advantages and solutions to some of the dilemmas that were associated with other technologies. The most important advantages are (I) access to the thoracic cavity through a nerveless area, and thus avoid the destruction of the intercostal nerves. This may surpass this technique on the other techniques that rely on the entrance to the thoracic cavity through an opening (or openings) in the intercostal spaces. (II) Subxiphoid approach provides a panoramic view of the anterior mediastinal space which enables the surgeon to see both phrenic nerves easily, in addition to the possibility to explore the neck and both pleural cavities easily so that all the important landmarks could be seen and explored from the middle line unlike the other unilateral approaches (24) (Figure 3A-D). (III) The cost of this technology is significantly lower than its robotics rival, which makes it easier to adopt and practice in any center so that it is not exclusive to large centers who contain a robotic device. (IV) The possibility of performing dual operations through one incision as pulmonary resections in addition to thymectomy without the need for additional incisions (25). In spite of all that has been said, however, the subxiphoid technique also has its weak points. The surgeon must have a previous practice and a thorough knowledge of the intercostal VATS before he can learn this type of operations. In addition to the need for a skilled and expert assistant surgeon, the lack of experience of the assistant surgeon in these operations may lead to increase the technical difficulties or even conversion or failure of the procedure. Anesthesia is an inseparable part of the surgical process and the development of the surgery towards the minimally invasive techniques must develop in parallel with minimally invasive anesthesia. The adoption of Pompeo and his colleagues (1) of the less invasive methods of anesthesia (non-intubated technique) is necessarily part of the future of thymus surgery. However, once entering the thoracic cavity through the intercostal space, the injury of the intercostal nerve during the operation is imaginable. In conclusion, the development of minimally invasive techniques for thymectomy has begun to enter multiple parallel routes. Although these techniques, which have both negatives and positives, vary, they eventually have to converge in one technique closer to the ideal in order to meet the needs of the surgeons and patients. In addition to the minimally invasive techniques of anesthesia, which may reduce morbidity significantly, There is no doubt that the robot has a big role in the future of surgeries, which has the advantages of the surgeon’s hands may be unable to compete, but the robot has to find the way to be affordable. In addition, the robot must be developed to be uniportal (this does not seem impossible).The subxiphoid technique appears to be exciting and catchy to most surgeons, but it is not as easy as it looks. Where the learning curve and difficulty of instrumentation may be a serious obstacle for those wishing to practice this technique. What is required here is the development of equipment to be more friendly and compatible to the surgeons’ hands, especially energy devices, which lack the angles required for this type of surgery. In order to reach the minimalist thoracoscopic resection of the thymus gland, a certain integration between robotics and subxiphoid techniques is necessary for the near future so that we can reach the optimum results.

Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by Section Editor Yun Che (Cancer Hospital of Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing, China).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2018.03.06). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pompeo E, Dauri M, Massa R, et al. Minimalist thoracoscopic resection of thymoma associated with myasthenia gravis. J Thorac Cardiovasc Surg 2017;154:1463-5. [Crossref] [PubMed]
- Blalock A, McGehee HA, Ford FR, et al. The treatment of myasthenia gravis by removal of the thymus gland preliminary report. JAMA 1941;117:1529-33. [Crossref]
- Masaoka A. Extended trans-sternal thymectomy for myasthenia gravis. Chest Surg Clin N Am 2001;11:369-87. [PubMed]
- Grandjean JG, Lucchi M, Mariani MA. Reversed-T upper mini-sternotomy for extended thymectomy in myasthenic patients. Ann Thorac Surg 2000;70:1423-4; discussion 1425. [Crossref] [PubMed]
- Calhoun RF, Ritter JH, Guthrie TJ, et al. Results of transcervical thymectomy for myasthenia gravis in 100 consecutive patients. Ann Surg 1999;230:555-9; discussion 559-61. [Crossref] [PubMed]
- Ando A, Azuma T, Aoe M, et al. Thoracoscopic extended thymectomy in conjunction with a collar incision of the neck for cases of myasthenia gravis. Kyobu Geka 1996;49:95-8. [PubMed]
- Novellino L, Longoni M, Spinelli L, et al. "Extended" thymectomy, without sternotomy, performed by cervicotomy and thoracoscopic technique in the treatment of myasthenia gravis. Int Surg 1994;79:378-81. [PubMed]
- Zieliński M. Technique of transcervical--subxiphoid-vats "maximal" thymectomy in treatment of myasthenia gravis. Przegl Lek 2000;57:64-5. [PubMed]
- Landreneau RJ, Dowling RD, Castillo WM, et al. Thoracoscopic resection of an anterior mediastinal tumor. Ann Thorac Surg 1992;54:142-4. [Crossref] [PubMed]
- Zahid I, Sharif S, Routledge T, et al. Video-assisted thoracoscopic surgery or transsternal thymectomy in the treatment of myasthenia gravis? Interact Cardiovasc Thorac Surg 2011;12:40-6. [Crossref] [PubMed]
- Pennathur A, Qureshi I, Schuchert MJ, et al. Comparison of surgical techniques for early-stage thymoma: feasibility of minimally invasive thymectomy and comparison with open resection. J Thorac Cardiovasc Surg 2011;141:694-701. [Crossref] [PubMed]
- Lin MW, Chang YL, Huang PM, et al. Thymectomy for non-thymomatous myasthenia gravis: a comparison of surgical methods and analysis of prognostic factors. Eur J Cardiothorac Surg 2010;37:7-12. [Crossref] [PubMed]
- Rückert JC, Ismail M, Swierzy M, et al. Minimally invasive thymus surgery. Chirurg 2008;79:18-20-5. [Crossref] [PubMed]
- Keating CP, Kong YX, Tay V, et al. VATS thymectomy for nonthymomatous myasthenia gravis: standardized outcome assessment using the myasthenia gravis foundation of America clinical classification. Innovations (Phila) 2011;6:104-9. [Crossref] [PubMed]
- Mineo TC, Pompeo E, Ambrogi V, et al. Adjuvant pneumomediastinum in thoracoscopic thymectomy for myasthenia gravis. Ann Thorac Surg 1996;62:1210-2. [Crossref] [PubMed]
- Liu Z, Yang J, Lin L, et al. Unilateral video-assisted thoracoscopic extended thymectomy offers long-term outcomes equivalent to that of the bilateral approach in the treatment of non-thymomatous myasthenia gravis. Interact Cardiovasc Thorac Surg 2015;21:610-5. [Crossref] [PubMed]
- Ng CS, Rocco G, Wong RH, et al. Uniportal and single-incision video-assisted thoracic surgery: the state of the art. Interact Cardiovasc Thorac Surg 2014;19:661-6. [Crossref] [PubMed]
- Wu CF, Gonzalez-Rivas D, Wen CT, et al. Single-port video-assisted thoracoscopic mediastinal tumour resection. Interact Cardiovasc Thorac Surg 2015;21:644-9. [Crossref] [PubMed]
- Rückert JC, Swierzy M, Ismail M. Comparison of robotic and nonrobotic thoracoscopic thymectomy: a cohort study. J Thorac Cardiovasc Surg 2011;141:673-7. [Crossref] [PubMed]
- Kido T, Hazama K, Inoue Y, et al. Resection of anterior mediastinal masses through an infrasternal approach. Ann Thorac Surg 1999;67:263-5. [Crossref] [PubMed]
- Zieliński M. Technique of transcervical-subxiphoid-VATS “maximal” thymectomy in treatment of myasthenia gravis. Przegl Lek 2000;57:64-5. [PubMed]
- Wu L, Lin L, Liu M, et al. Subxiphoid uniportal thoracoscopic extended thymectomy. J Thorac Dis 2015;7:1658-60. [PubMed]
- Suda T. Single-port thymectomy using a subxiphoid approach-surgical technique. Ann Cardiothorac Surg 2016;5:56-8. [PubMed]
- Akar FA. Subxiphoid Uniportal Approach is it Just a Trend or the Future of VATS. MOJ Surg 2017;4:00076.
- Argueta AJ, Cañas SR, Abu Akar F, et al. Subxiphoid approach for a combined right upper lobectomy and thymectomy through a single incision. J Vis Surg 2017;3:101. [Crossref] [PubMed]
Cite this article as: Abu Akar F, Shaqqura BH, Gonzalez-Rivas D. Editorial on minimalist thoracoscopic resection of thymoma associated with myasthenia gravis. Mediastinum 2018;2:22.