Transcervical thymectomy
Introduction
Historically, transcervical thymectomy was the first technique of intentional resection of the thymus in patient suffering from myasthenia gravis (MG). Such procedure was performed in 1911 by Sauerbruch, the father of thoracic surgery, who performed transcervically a partial thymectomy and a partial thyroidectomy in the patient suffering from the Graves-Basedow disease associated with MG, with subsequent clinical improvement of MG (1). Afterwards, the transsternal approach for thymectomy of thymomas and MG was introduced by Blalock in 1939 (2). However, transcervical thymectomy was restored by Crile and the other surgeons from 1965 as a less invasive procedure than a transsternal thymectomy, which was a standard in that time (3-5). Thymectomy performed through a cervical approach was a partial/subtotal resection of the gland (6). A further step was of development of the technique of transcervical extended thymectomy with lifting of the sternum with the Cooper retractor (7). This procedure enabled complete resection of the thymus together with the fatty tissue surrounding the gland. However, transcervical thymectomy never gained a wider acceptance, despite the claims of the proponents of this procedure, that late results of treatment in terms of complete remission rate of MG have been equivalent to transternal extended thymectomy (8,9). The possible advantages of the transcervical thymectomy are an extremely short hospital stay, no need for chest drainage and lack of long-lasting pain caused by the incision placed in the neck (10). Besides, transcervical approach may also be a part of a combined procedure as was described by Jaretzki, who used a transsternal incision supplemented with cervical incision to enable complete radical resection of the superior poles of the gland and removed the adipose tissue of neck, possibly containing ectopic thymic centers for increased chance for complete remission of MG (11). Maggi et al. performed a collar incision in the neck with an upper partial sternotomy hidden behind the dissected flap of soft tissue of the anterior chest to gain a better access to the thymus (12). Novellino et al combined cervical incision with lifting of the sternum and three-port video-thoracoscopy (VATS) on each side of the chest. This procedure was later described as a Video-Assisted Thoracoscopic Extended Thymectomy (VATET) (13). Our team introduced a technique of transcervical-subxiphoid-VATS maximal thymectomy combining transcervical and subxiphoid approaches with lifting of the sternum from above (the manubrium) and from below (the lower sternal angle) supplemented with bilateral one-port VATS (14). Similar technique was described by Takeo et al. (15). Shiono et al. recognized the value of transcervical approach as a supplementation of a VATS thymectomy due to incompleteness of resection of the superior thymic poles by VATS (16). Cooper and Keshavjee introduced the technique of transcervical thymectomy under control of VATS, with introduction of the thoracoscope through the cervical wound (17,18). Sukumar et al. combined transcervical thymectomy with deliberate opening of pleural cavities for introduction of VATS through the transcervical incision to facilitate dissection under VATS control (19).
Methods
Patient selection and workup
At our institution only selected patients with small thymic tumors without MG (little risk of thymoma) or high operative risk due to severe co-morbidities are candidates for transcervical thymectomy.
For all patients with nonthymomatous MG with or without thymomas our procedure of choice is the subxiphoid-VATS extended thymectomy. For patients with advanced stage III thymomas we choose the transsternal approach.
At some other institutions transcervical thymectomy is used for patients’ small thymomas with/without MG.
The contraindications for transcervical thymectomy include excessive obesity, stiffness of the cervical spine, prior mediastinal surgery (e.g., cardiac operation). Another limitation for this kind of procedures are dimensions of the thymic tumor above 4–5 centimeters (5,10). For patients with MG without thymoma an option of direct thymectomy is possible in patients with a mild or moderate disease (the MGFA class I–IIIb; mild to moderate ocular, bulbar and extremities muscles affected) (20). In patients with severe MG symptoms the optimal solution is to defer the time of surgery to giver the patient enough time to get better after therapy these steroids, immunosuppressive drugs, plasmapheresis or immunoglobulins.
Description of the approach (pre-operative preparation and equipment preference card):
- The Zakopane bar with a single-tooth hook (BBraun, Aesculap-Chifa, Nowy Tomysl, Poland);
- The advanced cautery device—Bi-clamp, Harmonic knife or Ligasure;
- The Cameleon videothoracoscope (KARL STORZ GmbH & Co. KG, Tuttlingen, Germany);
- Standard open-surgery and VATS instruments.
Procedure
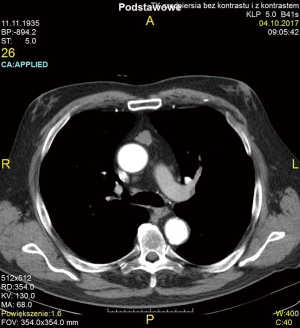
The case of 82 years old patients with a thymic tumor (Figure 1) with associated MG is presented below.
Technique of transcervical thymectomy
A collar 8 cm incision in the neck was done in the crease, little above the sternal notch. The anterior jugular veins were cut and secured with suture-ligation. The median raphe between the strap muscles was cut and the muscles were retracted laterally. The thyroid gland was bluntly dissected and both laryngeal recurrent nerves are shown with much attention paid to avoid their injury (Figure 2). A one-tooth hook attached to the Zakopane bar (BBraun, Aesculap-Chifa, Nowy Tomysl, Poland) was introduced under the manubrium of the sternum in aim to elevate it for several centimeters to facilitate an adequate access to the anterior mediastinum. The thymus gland is resected en-bloc with the surrounding fatty tissue of the lower neck and the anterior superior mediastinum. The inferior thyroid veins and the thymic veins draining blood from the thymus to the left innominate vein are secured with vascular clips and divided—the other methods to secure these vessels are a harmonic knife or ligasure. For better control, a video-thoracoscope (VATS) is inserted to the mediastinum through the cervical incision. The lowers poles of the thymus are separated from the pericardium and the specimen is removed. Usually, the right lower pole is dissected first and the left lower pole is managed during further dissection of the aortopulmonary window is a difficult, but very important part of transcervical thymectomy. Hemostasis was checked and pieces of Spongostan were inserted to the mediastinum for additional security. No drain was left in the mediastinum and the patient was extubated directly after surgery. In most of cases the postoperative course is usually uneventful. However, the presented patient had a difficult postoperative course and necessitated intubation and the use of ventilator for 7 days for myasthenic crisis. Subsequently the patients recovered. There were no surgical complications. On final pathology there was no thymoma.

Tips, tricks and pitfalls
Complete or extended transcervical thymectomy is virtually impossible without elevation of the sternum.
- The main advantages of a transcervical thymectomy are a lack of persistent pain after procedure, no necessity for chest drainage and no violation of the pleural cavities.
- The disadvantages include:
- Poor cosmetic result due a scar in a visible place in the neck, especially important in the population including mainly young women.
- More serious drawback is a low extensiveness of a transcervical thymectomy, which precludes radical resection of the adipose tissue of the middle and lower anterior mediastinum.
- The use of VATS technique in the superior mediastinum approached from the neck is very difficult due to the limited space created during dissection. These difficulties, which are especially pronounced in obese patients with short neck and barrel-shaped chest, are very clearly seen on the attached video.
- For the transcervical approach it is virtually impossible to excise mediastinal tissue from the level of the thoracic outlet down to the diaphragm without opening of the pleural spaces and introduction of a thoracoscope.
- In case of deliberate wide opening of the unilateral or bilateral mediastinal pleura insertion of the chest tube to one or both pleural cavities is necessary, which eliminates one of the potential advantages of transcervical approach (see above).
- Overall, transcervical thymectomy is much inferior to the subxiphoid one, both in terms of extensiveness and technical ease of the procedure.
Results
There were 18 patients (2 for MG with associated thymic tumors and 16 for the tumors/cysts of the anterior mediastinum without MG) in the period 1/1/2009 to 31/12/2017. The morbidity was 5.6%, with no mortality. The mean time of the procedure was 105.4 min. (45–150 min).
Conclusions
The transcervical approach combined with VATS and lifting of the sternum facilitates thymectomy in case of small thymic tumors with/without MG. This technique is more difficult and less extensive that subxiphoid thymectomy.
Acknowledgments
We are grateful to Mr. Michael Clark for reviewing the manuscript.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors Nuria Novoa and Wentao Fang for the series “Minimally Invasive Thymectomy” published in Mediastinum. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2018.03.09). The series “Minimally Invasive Thymectomy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board and the informed consent was obtained from every patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Keesey JC. A history of treatments for myasthenia gravis. Semin Neurol 2004;24:5-16. [Crossref] [PubMed]
- Blalock A, Mason MF, Morgan HJ, et al. Myasthenia gravis and tumors of the thymic region: report of a case in which the tumor was removed. Ann Surg 1939;110:544-61. [Crossref] [PubMed]
- Kark AE, Kirschner PA. Total thymectomy by the transcervical approach. Br J Surg 1971;58:321-6. [Crossref] [PubMed]
- Kirschner PA. The history of surgery of the thymus gland. Chest Surg Clin N Am 2000;10:153-65. x. [PubMed]
- Papatestas AE, Pozner J, Genkins G, et al. Prognosis in occult thymomas in myasthenia gravis following transcervical thymectomy. Arch Surg 1987;122:1352-6. [Crossref] [PubMed]
- Papatestas AE, Genkins G, Kornfeld P, et al. Effects of thymectomy in myasthenia gravis. Ann Surg 1987;206:79-88. [Crossref] [PubMed]
- Cooper JD, Al-Jilaihawa AN, Pearson FG, et al. An improved technique to facilitate transcervical thymectomy for myasthenia gravis. Ann Thorac Surg 1988;45:242-7. [Crossref] [PubMed]
- de Perrot M, Bril V, McRae K, et al. Impact of minimally invasive trans-cervical thymectomy on outcome in patients with myasthenia gravis. Eur J Cardiothorac Surg 2003;24:677-83. [Crossref] [PubMed]
- DeFilippi VJ, Richman DP, Ferguson MK. Transcervical thymectomy for myasthenia gravis. Ann Thorac Surg 1994;57:194-7. [Crossref] [PubMed]
- Shrager JB, Deeb ME, Mick R, et al. Transcervical thymectomy for myasthenia gravis achieves results comparable to thymectomy by sternotomy. Ann Thorac Surg 2002;74:320-6; discussion 326-7. [Crossref] [PubMed]
- Jaretzki A 3rd, Bethea M, Wolff M, et al. A rational approach to total thymectomy in the treatment of myasthenia gravis. Ann Thorac Surg 1977;24:120-30. [Crossref] [PubMed]
- Maggi G, Casadio C, Cavallo A, et al. Thymectomy in myasthenia gravis. Results of 662 cases operated upon in 15 years. Eur J Cardiothorac Surg 1989;3:504-9; discussion 510-1. [Crossref] [PubMed]
- Novellino L, Longoni M, Spinelli L, et al. "Extended" thymectomy, without sternotomy, performed by cervicotomy and thoracoscopic technique in the treatment of myasthenia gravis. Int Surg 1994;79:378-81. [PubMed]
- Zieliński M. Technique of transcervical--subxiphoid-vats "maximal" thymectomy in treatment of myasthenia gravis. Przegl Lek 2000;57:64-5. [PubMed]
- Takeo S, Sakada T, Yano T. Video-assisted extended thymectomy in patients with thymoma by lifting the sternum. Ann Thorac Surg 2001;71:1721-3. [Crossref] [PubMed]
- Shiono H, Shigemura N, Okumura M. Inclusion of the transcervical approach in video-assisted thoracoscopic extended thymectomy (VATET) for myasthenia gravis: a prospective trial. Surg Endosc 2008;22:1135-6. [Crossref] [PubMed]
- Donahoe L, Keshavjee S. Video-assisted transcervical thymectomy for myasthenia gravis. Ann Cardiothorac Surg 2015;4:561-3. [PubMed]
- Calhoun RF, Ritter JH, Guthrie TJ, et al. Results of transcervical thymectomy for myasthenia gravis in 100 consecutive patients. Ann Surg 1999;230:555-9; discussion 559-61. [Crossref] [PubMed]
- Komanapalli CB, Person TD, Schipper P, et al. An alternative retractor for transcervical thymectomy. J Thorac Cardiovasc Surg 2005;130:221-2. [Crossref] [PubMed]
- Jaretzki A 3rd, Barohn RJ, Ernstoff RM, et al. Myasthenia gravis: recommendations for clinical research standards. Task Force of the Medical Scientific Advisory Board of the Myasthenia Gravis Foundation of America. Ann Thorac Surg 2000;70:327-34. [Crossref] [PubMed]
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. The procedure of transcervical thymectomy. Asvide 2018;5:384. Available online: http://www.asvide.com/article/view/24000
Cite this article as: Zieliński M, Rybak M, Solarczyk-Bombik K, Wilkojc M, Czajkowski W, Kosinski S, Fryzlewicz E, Nabialek T, Szolkowska M, Pankowski J. Transcervical thymectomy. Mediastinum 2018;2:28.