Video-assisted thoracic surgery thymectomy: subxiphoid approach
Introduction
The goal of this paper is to describe the technique and advantages of subxiphoid approach for thymomatous and non-thymomatous myasthenia gravis (MG).
The first publication on a subxiphoid thymectomy was made by Ito et al. (in Japanese, but abstract in English and very instructional photographs and figures), mentioned by Kido et al. (1,2). Ito et al. combined a cervical and subxiphoid incision, elevated the sternum with a tape and removed the thymus with the anterior mediastinal fat tissue with aid of mediastinoscope. The operation lasted 5.5 hours and there was hardly any postoperative pain due to the sternum elevation and mediastinal maneuvers.
There are at least two reasons to perform thymectomy through a subxiphoid incision, which has been also described as an infrasternal. First of all, contrary to unilateral video-assisted thoracic surgery (VATS) technique, a subxiphoid approach allows for visualization and access to both sides of the mediastinum, including both phrenic nerves, which is critically important for radical en bloc resection of the entire thymus with the surrounding mediastinal—pleura and the fat of the mediastinum and the lower neck region.
Due to elevation of the manubrium in a patient in a supine position it is feasible to continue dissection high up to the level of thyroid, which permits for complete resection of the uppermost parts of the thymic poles. Such completeness is rather impossible for the VATS approach (even with bilateral VATS). The second, very important advantage of a subxiphoid incision is much less pain caused by a subxiphoid incision in comparison to VATS, due to avoidance of the intercostal nerve injury during intercostal incisions.
The shape of operative wound in case of the transverse subxiphoid incision with lifting of the lower sternal angle becomes round or oval spade, which enables removal of even quite large diameter thymic tumors through this incision. Contrary to the VATS intercostal incisions, in case of a subxiphoid incision there are no ribs, which could restrict an access to the chest. The biggest thymic tumor, which was completely removed at our institution, had a diameter of 14 centimeters.
There are numerous technical sub-types of the subxiphoid thymectomy, which include a sole subxiphoid access, with or without lifting of the sternum; uniportal or combined with VATS (with intercostal or subcostal ports) and/or transcervical incision; with/without the use CO2 insufflation (3-10). A subxiphoid incision may be transverse or longitudinal in the midline; with/without resection of the xiphoid process. A procedure can be performed with a VATS or robotic [robotic-assisted thoracic surgery (RATS)] technique (11). A scope of removal of the mediastinal tissue surrounding of the thymus gland may decide if the procedure is a basic one (resection of the thymus gland, only), extended (resection of the gland along with the fat of the anterior mediastinum) or, so-called the maximally extended one (12).
Methods
Patient selection and workup and pre-operative preparation
Every patient with MG without thymoma or with clinical early-stage T1–2 and some T3 thymomas is a good candidate for such operation (13). For the advanced stage T3–4 thymic tumors the optimal approach is through a median sternotomy, usually with use of neoadjuvant chemo-radiotherapy. In patients with MG without thymoma the operation is offered in case of a stable disease (12). In patients with a clinically unstable myasthenia the operation is hold off and the myasthenia is treated with steroids, immunosuppressive drugs, plasmapheresis or immunoglobulins until a substantial clinical improvement in noted. Otherwise, there is high risk of postoperative myasthenic crisis.
Equipment preference card
- The Zakopane frame with two hooks;
- Bi-clamp, harmonic knife or ligasure;
- The Yankauer suction tube;
- EndoCAMeleon® telescope with variable direction of view (Karl Storz);
- Standard VATS instruments.
Surgical technique of the uniportal subxiphoid-VATS extended thymectomy
A patient is lying supine on an operating table with elevation of the chest and hyperextension of the neck. Selective endobronchial intubation enables possibility of one-lung ventilation, if necessary
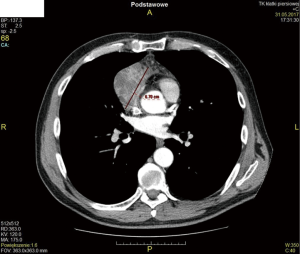
A or longitudinal 5–7 cm incision is done over the xiphoid process (Figure 1). An extent of incision is dependent on the build of the body. If a transverse incision is chosen the medial edges of the rectus muscles are divided down to the level of the costal arches. For a longitudinal incision the abdominal fascia is cut in the midline. In the presented video a midline longitudinal 8 cm incision was made, which was longer than usually done, due to the large size of the tumor measuring 10 cm × 7 cm × 6 cm (Figures 2,3). The xiphoid process is removed when is ossified (as was done in the presented operation) or, in case of a soft chondral xiphoid it is spared. Generally, a single left lung ventilation is commenced to cause a collapse of the right lung or, in some patients, a two-lung ventilation with some permissive hypoventilation is accepted. A sternal hook connected to the Zakopane frame is put underneath the lower sternal angle, which is subsequently lifted to improve access to the chest. The right mediastinal pleura is cut and the EndoCAMeleon® videothoracoscope is introduced to the right chest cavity. The entire dissection is performed with a cautery device (bipolar electrocautery, harmonic knife or ligasure).

Both pleural cavities are opened by cutting the mediastinal pleura close to the internal surface of the sternum. Care must be paid to avoid injury of the mammary vessels. The dissected mediastinal structures are pressed towards the spine with the Yankauer suction tube for protection while the second single-tooth hook is inserted percutaneously beneath the manubrium through a 2–3 mm puncture made over the sternal notch (Figure 4). Lifting of the sternum with both hooks enhances the view of the structures of the upper mediastinum and the lower neck and permits for reaching of the level of the connection between the superior thymus and the lower poles of the thyroid gland. En bloc dissection of the specimen starts from the prepericardial fat and the right and left epiphrenic fat pads which are disconnected from the diaphragm and the pericardium. The specimen including the prepericardial fat, the thymic tumor and the thymus gland is continued in the cephalad direction under control of a videothoracoscope (Figure 5). The phrenic nerves are the margins of dissection. Thymic veins (usually more than one) are closed with vascular clips and cut sequentially close to the left innominate vein until the left internal thoracic vein (left mammary vein) is reached and spared. Due to opening of both pleural cavities it is possible to transfer of the dissected specimen obscuring plane of dissection from one pleural cavity to the other, when necessary. This maneuver enhances an operation considerably due to the better view of the dissection planes. The lower thyroid veins are managed in the similar way as the thymic veins. Further dissection proceeds along the thymic poles until the lower part of the thyroid is clearly visualized (Figure 6). The upper poles or the thyro-thymic ligaments are disconnected proximally to the thyroid. In the course of the operation such anatomical structures as the innominate artery, the right carotid arteries and the trachea are clearly displayed. The freed upper poles of the thymus are retracted in the cephalad direction for completion of dissection of the specimen from the pericardium. The left mediastinal pleura is cut along the left phrenic nerve, in the similar way as on the right side. The specimen including the thymus with a tumor and the adipose tissue is put into an endo-bag and removed through the incision. The final step of the procedure in a dissection of the aorta-pulmonary window.

Haemostasis is proofed and a single Ch 24–28 chest tubes are inserted into each pleural cavity through the uniportal incision. Ventilation of both lungs is resumed. The subxiphoid incision is sutured in the standard technique, a puncture incision is managed with a single 5/0 suture which is substituted with a peristrip on the following day.
Post-operative management
As a general rule, a patient is extubated soon after completion of the procedure. If the patient takes steroids and/or immunosuppressive this therapy is re-started without delay. The anticholinesterase drugs are given in the preoperative doses as soon as the clinical symptoms of MF relapse which may take several hours or several days. In some rare cases there is no need to give these kinds of drugs postoperatively (immediate clinical remission). Chest tubes are usually removed on the first or second postoperative day and duration of postoperative hospitalization is 4–7 days.
Tips, tricks and pitfalls
- A transverse subxiphoid incision should be performed just below the junction of the lower angle of the sternum and the xiphoid process. The length of the incision is dependent on the patients’ body structure—in case of slender patients with non-thymomatous MG, a 3-cm incision could provide a satisfactory access, contrary to the 5–8 cm incision which might be necessary for obese patients or in case of larger tumors. In case of a longitudinal midline approach the length of incision is similar;
- It is useful to ask an anesthesiologist to ventilate both lungs with relatively small volumes to allow simultaneous access to both pleural cavities. The initial next step is a division of the anterior mediastinal pleura membranes to open both pleural spaces;
- Afterwards, the right and the left epiphrenic fat pads are disconnected from the diaphragm and the pericardium. Dissection of the specimen including the whole thymus gland continues in the cephalad direction. In case of obese patients and especially in thymomas it is useful to open the mediastinal pleura to transfer the specimen to the contralateral left pleural cavity. This maneuver gives the clear view of the plane of dissection and enhances facilitates dissection of the specimen from the pericardium;
- Dissection on the right it is enhanced by rotation an operating table to the left and in the opposite direction during dissection on the left side;
- Dissection of the superior mediastinal and lower neck areas located cranially to the left innominate vein are the most demanding parts of the operation. The goal is to show lower poles of the thyroid gland to remove completely the upper poles of the thymus and the surrounding fatty tissue. The innominate artery, right and left carotid arteries and the trachea should be clearly dissected. This can be achieved with the simultaneous use of the bipolar electrocautery (or harmonic knife or ligasure) and the Yankauer suction tube which is used to dissect and retract tissue. Avoidance of injury of the left recurrent nerve which might occur during dissection in the area located on the left side of the trachea is a priority;
- Dissection of the adipose content of the aorta-pulmonary window is completed after removing of specimen from the chest. A proper dissection of this area should allow for visualization of the left pulmonary artery and the left vagus nerve, which confirms that whole content of the aorta-pulmonary window has been completely removed.
Results
The results of the whole group of patients in whom the subxiphoid approach was used for thymectomy are summarized in Table 1. The entire group of patients in whom the subxiphoid approach was used for thymectomy included 611 patients, overall (80 patients with thymomas, 516 patients with non-thymomatous MG and 15 patients with repeated thymectomy) operated on from Sep 2000 to Sep 2017. There were 5 uniportal subxiphoid-VATS extended thymectomies (for non-thymomatous MG in 2 patients and for thymic tumors in 2 patients). The mean operative time was 118.5 min (range, 85–130 min). For the whole group of 606 patients there was no mortality and less than 5% morbidity. The complete remission rate 53.1% for the transcervical-subxiphoid-VATS maximal thymectomy approach for non-thymomatous MG was reported (18).
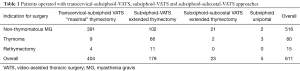
Full table
Conclusions
The subxiphoid uniportal incision with sternal lifting facilitates performance of extended thymectomy for thymomas or MG without thymoma.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors Nuria Novoa and Wentao Fang for the series “Minimally Invasive Thymectomy” published in Mediastinum. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2018.05.03). The series “Minimally Invasive Thymectomy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board (No. 1/2018) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kido T, Hazama K, Inoue Y, et al. Resection of anterior mediastinal masses through an infrasternal approach. Ann Thorac Surg 1999;67:263-5. [Crossref] [PubMed]
- Ito S, Tagawa T, Ide S, et al. Mediastinoscopic Extended thymectomy using a sternum lifting method. J Jpn Assoc Chest Surg 1997;11:181-5. [Crossref]
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Subxiphoid thymectomy - technical variants. Video-assist Thorac Surg 2017;2:9. [Crossref]
- Zieliński M. Technique of transcervical-subxiphoid-VATS “maximal” thymectomy in treatment of myasthenia gravis. Przegl Lek 2000;57:64-5. [PubMed]
- Takeo S, Sakada T, Yano T. Video-assisted extended thymectomy in patients with thymoma by lifting the sternum. Ann Thorac Surg 2001;71:1721-3. [Crossref] [PubMed]
- Uchiyama A, Shimizu S, Murai H, et al. Infrasternal mediastinoscopic thymectomy in myasthenia gravis: surgical results in 23 patients. Ann Thorac Surg 2001;72:1902-5. [Crossref] [PubMed]
- Hsu CP. Subxiphoid approach for thoracoscopic thymectomy. Surg Endosc 2002;16:1105. [Crossref] [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
- Dunning J. Video-assisted thoracoscopic microthymectomy. Ann Cardiothorac Surg 2015;4:550-5. [PubMed]
- Zhao J, Wang J, Zhao Z, et al. Subxiphoid and subcostal arch thoracoscopic extended thymectomy: a safe and feasible minimally invasive procedure for selective stage III thymomas. J Thorac Dis 2016;8:S258-64. [PubMed]
- Suda T, Kaneda S, Hachimaru A, et al. Thymectomy via a subxiphoid approach: single-port and robot-assisted. J Thorac Dis 2016;8:S265-71. [PubMed]
- Jaretzki A 3rd, Barohn RJ, Ernstoff RM, et al. Task Force of the Medical Scientific Advisory Board of the Myasthenia Gravis Foundation of America: Myasthenia gravis: recommendations for clinical research standards. Ann Thorac Surg 2000;70:327-34. [Crossref] [PubMed]
- Nicholson AG, Detterbeck FC, Marino M, et al. The IASLC/ITMIG thymic epithelian tumors staging project: proposal for the T component for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S73-80. [Crossref] [PubMed]
- Zieliński M, Gwozdz P, Solarczyk-Bombik K, et al. Subxiphoid incision, elevation of the sternum, opening of the right mediastinal pleura, dissection of the right epiphrenic fat pad from the diaphragm and the pericardium. Asvide 2018;5:564. Available online: http://www.asvide.com/article/view/25326
- Zieliński M, Gwozdz P, Solarczyk-Bombik K, et al. Dissection of the left epiphrenic fat pad from the diaphragm and the pericardium, dissection of the thymoma and the mediastinal tissue from the sternum, introduction of the upper sternal hook, dissection of the specimen from the left phrenic nerve and the pericardium. Asvide 2018;5:565. Available online: http://www.asvide.com/article/view/25327
- Zieliński M, Gwozdz P, Solarczyk-Bombik K, et al. Dissection of the specimen from the right phrenic nerve and the pericardium, clipping and division of the thymic and lower thyroid veins. Asvide 2018;5:566. Available online: http://www.asvide.com/article/view/25328
- Zieliński M, Gwozdz P, Solarczyk-Bombik K, et al. Dissection of the right and left lobes of the thyroid gland, the lower thyroid vein, the trachea and the thymic vein, extraction of the specimen from the chest, view of the specimen including thymoma, dissection of the aorta-pulmonary window. Asvide 2018;5:567. Available online: http://www.asvide.com/article/view/25329
- Zielinski M, Hauer L, Hauer J, et al. Comparison of complete remission rates after 5 year follow-up of three different techniques of thymectomy for myasthenia gravis. Eur J Cardiothorac Surg 2010;37:1137-43. [Crossref] [PubMed]
Cite this article as: Zieliński M, Gwozdz P, Solarczyk-Bombik K, Wilkojc M, Czajkowski W, Kosinski S, Fryzlewicz E, Nabialek T, Szolkowska M, Pankowski J. Video-assisted thoracic surgery thymectomy: subxiphoid approach. Mediastinum 2018;2:45.