
Middle mediastinal paraganglioma with blood supply by branch of left coronary artery: one case report
Introduction
Paragangliomas are neuroendocrine tumors arising from extra-adrenal paraganglions of the autonomic nervous system while mediastinal paragangliomas are thought to deriving from para-aortic and para-vertebral chromaffin tissues. Based on the catecholamine metabolism and secretion, they are divided into functional or nonfunctional groups. Although most mediastinal paragangliomas are nonfunctional, catecholamine hypersecretion or compression by some functional tumors can also lead to hoarseness, dyspnea, and chest pain (1). The middle mediastinal location is extremely rare. The management currently rely on complete surgical resection because of special anatomical position and relatively resistant to chemotherapy and irradiation (2,3).
Case presentation
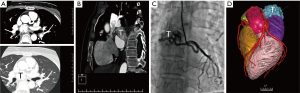
A 40-year-old female patient was referred because of repeated palpitation. Echocardiography and chest computed tomography (CT) showed a lesion in the mediastinum and left atrium suspicious for a neuroendocrine tumor. The tumor localized at middle mediastinal right front of esophagus, measuring about 4 cm in diameter. Coronarography confirmed the branch of left coronary artery as the feeding vessel of the tumor. Three-dimensional reconstruction image displayed the mass was closely adherent to the pericardium (see in Figure 1). Intraoperative exploration detected a well-circumscribed mass located at the top of the left atrium placeholder and firmly fixed to the myocardium. Under general anesthesia, a complete resection was performed and the left atrial wall was rebuilt by autologous pericardium piece. Electrocardiogram showed no abnormality in contractile activity of left ventricle at all stages under resting state before surgery. Three days after surgery, cardiac ultrasonography showed a small amount of pericardial effusion. Cardiac ultrasonography showed a mild regurgitation of the mitral valve 22 days after surgery.
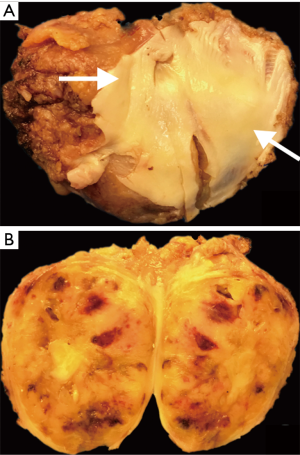
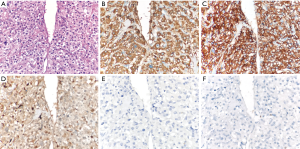
Gross photograph view of the resected mass showed a well-circumscribed soft tumor attached by a piece of pericardium. The cut surface was homogeneous admixed with hemorrhagic areas (see in Figure 2). Histopathological examination showed typical organoid pattern and highly vascular nature. Necrosis or vascular invasion were not encountered and immunohistochemical stains confirmed a paraganglioma diagnosis with synaptophysin, S100 and chromogranin-A positivity, pCK, desmin and TFE-3 negativity and a 2% index of proliferation (Ki-67) (see in Figure 3). Follow-up information had so far been shown no evidence of complication or recurrence after 25 months of surgical resection until now.
Discussion and conclusions
We present a 40-year-old woman with a middle mediastinal mass that was fed by branch of left coronary artery, and was finally diagnosed as primary mediastinal paragangliomas without an adrenal lesions. Serum and 24-hour urinary biochemical markers showed no elevated catecholamines and chromogranin A levels, consistent with a non-functional paraganglioma. Besides, it was unreliable to predict biologic behavior from the perspective of morphology. And finally, the mass was dissected off the myocardium and freed from surrounding soft tissue with well-defined margins. There was no evidence of recurrence or adrenal and ex-adrenal occupied lesion after surgical resection.
This study was approved for review by the ethics committee (informed consent for patient biopsy) of Shanghai Chest Hospital of Shanghai Jiao Tong University. And the ID/number of ethics approval was KS1350.
Written informed consents were obtained from this patient before surgery and for publication of case report in succession.
Acknowledgments
We want to thank Dr. Jing chen and Prof. Busheng Zhang (Department of Imaging and Cardiothoracic surgery, Shanghai Chest Hospital) for their interpretation and knowledge of imaging and surgery.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2018.07.04). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Brown ML, Zayas GE, Abel MD, et al. Mediastinal paragangliomas: the mayo clinic experience. Ann Thorac Surg 2008;86:946-51. [Crossref] [PubMed]
- Takashima Y, Kamitani T, Kawanami S, et al. Mediastinal paraganglioma. Jpn J Radiol 2015;33:433-6. [Crossref] [PubMed]
- Wald O, Shapira OM, Murar A, et al. Paraganglioma of the mediastinum: challenges in diagnosis and surgical management. J Cardiothorac Surg 2010;5:19. [Crossref] [PubMed]
Cite this article as: Zhao J, Zhu L, Yu K, Zhang J, Han Y. Middle mediastinal paraganglioma with blood supply by branch of left coronary artery: one case report. Mediastinum 2018;2:48.


