
Video-assisted mediastinoscopic lymphadenectomy combined with transcervical thoracoscopy
Introduction
The purpose of surgical staging of lung and pleural cancers is planning treatment and assessing prognosis.
Transcervical video-mediastino-thoracoscopy (VMT) (1,2) allows access to the mediastinum and one or both pleural cavities. It facilitates to identify the cell type and stage in lung cancer and other thoracic malignancies, such as mesothelioma (3).
Surgical explorations have the highest certainty (4) before lung or pleural resection.
Video-assisted mediastinoscopic lymphadenectomy (VAMLA) (5-8) is a completely endoscopic procedure performed with the two-valved video-mediastinoscope. It consists of complete lymphadenectomy (including fatty tissue and lymph nodes) of the subcarinal, the right paratracheal and the left paratracheal space- nodal stations 7, 4R and 4L, respectively, according to the International Association for the Study of Lung cancer lymph node map (4,9). In the left paratracheal space we need to be careful not to injury left recurrent nerve. Once right paratracheal lymphadenectomy is completed allows us to identify and incise the right mediastinal pleural. Once it is opened, a 30º-5 mm thoracoscope is introduced through the video-mediastinoscope. With the 30º video-thoracoscope we can explore both pleural cavities and the lung surface. If we identify pleural or lung nodules, biopsies can be taken to confirm or discard tumour dissemination. To access to the left pleural cavity, VAMLA is combined with extended mediastinoscopy, the route of which over the aortic arch is used to access the left mediastinal pleura (10-12).
With this procedure, the mediastinum and the pleural cavities are explored from a single cervical incision and in the same surgical setting, widening the range of the explorations and improving the staging of thoracic malignancies (13,14). It is especially indicated in the next situations:
- Patients with lung cancer associated with pleural effusion with negative cytology by thoracocentesis and no lymph node involvement in PET/CT scan but there are other criteria for mediastinal staging (15).
- Patients with mesothelioma but the histological subtype (epithelioid, biphasic and sarcomatoid) is unknown or mediastinal staging is required.
- Pleurodesis for symptomatic control of malignant pleural effusions.
- Pulmonary nodules detected during the exploration can be resected (13).
Operative techniques
Patient’s position and anaesthetic considerations
The patient is in supine position with a sandbag placed between the scapule. It allows to achieve the maximal neck hyperextension. The head is supported on a head ring.
One of the differences with standard VAMLA is that a single-lung ventilation with a double- lumen tube is needed to complete the exploration of pleural cavity (Figure 1).
Instrumentation
We recommend to use the Linder-Dahan spreadable video-mediastinoscope (Richard Wolf, Knittlingen, Germany) instead of Lerut DCI video mediastinoscope (KARL STORZ SE & Co. KG, Tuttlingen, Germany) because it allows to enlarge the operative field creating an optimal exposure of the mediastinum.
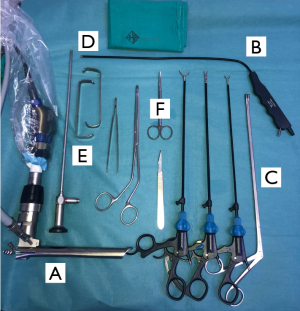
Regarding instrumentation, the same standard mediastinoscopy instruments can be used (Figure 2). A 5 mm video-thoracoscope is used to explore the pleural cavity. A 30º viewing provides a panoramic view.
Biopsies of parietal pleural can be performed with the same forceps used during VAMLA. If pleural effusion is identified during thoracoscopy, we should take samples for cytological and biochemical analyses.
Surgical procedure
Incision
A cervical incision is performed over the sternal notch (Figure 3). The subcutaneous tissue and the platysma are incised, the paratracheal muscles are separated laterally and the pretracheal fascia is incised. Then, a pretracheal space is created by digital dissections. This space is necessary to insert the video-mediastinoscope into the mediastinum (Figure 4).
VAMLA steps
Subcarinal lymphadenectomy
Subcarinal nodes are completely excised following the landmarks, along the main bronchi, the pulmonary artery and the oesophagus. Like you see in Figure 5, when the subcarinal nodes are excised en bloc, the upper part of the para-oesophageal lymph nodes can be excised, too.

Right paratracheal lymphadenectomy
The right inferior paratracheal nodes are totally excised down to the azygos vein and right main bronchus.
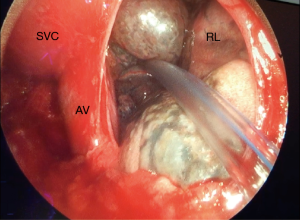
Once lymphadenectomy is completed the superior vena cava and the right mediastinal pleura are exposed (Figure 6).

Left paratracheal lymphadenectomy
First of all, the left recurrent laryngeal nerve is identified and then the left inferior paratracheal nodes are carefully dissected and removed individually. To explore subaortic and para-aortic nodes in left lung cancers, extended cervical video-mediastinoscopy or parasternal mediastinotomy should be added (10) (Figure 7).

Transcervical thoracoscopy
Right transcervical thoracoscopy
The 5 mm 30º video-thoracoscope is introduced through the valves of the video-mediastinoscope (Figures 8,9).
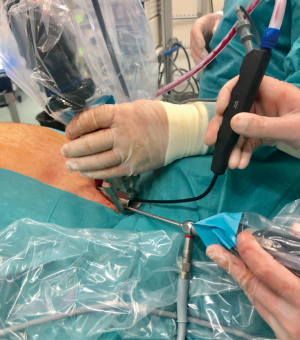
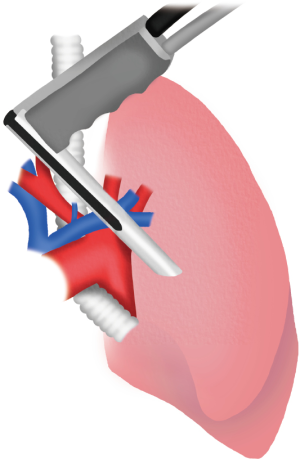
After removing the right inferior paratracheal lymph nodes, the mediastinal pleura is grasped and incised. The ipsilateral lung is collapsed and the video-thoracoscope is introduced to the pleural cavity. With a second screen connected to the video-thoracoscope, the entire pleural cavity is explored. The parietal or visceral pleura and lung nodules if present can be biopsied. The opening of the two-valved video-mediastinoscope even allows the insertion of endoscopic staplers to perform wedge resections of the lung (13) (Figure 10).

Left transcervical thoracoscopy (Figure 11
To explore the left pleural cavity is necessary to create a tunnel by digital blunt dissection. By the same cervical incision, this tunnel is created between the innominate artery and the left carotid artery moving above the aortic arch and under the left innominate vein.
Once the mediastinal pleura is identified we can perform a pleurotomy under direct endoscopic view to examine the left pleural cavity (20).
Assouad et al. described a new approach to the left pleural cavity passing through the retrosternal space. To complete the thoracoscopy they used a flexible endoscope through the valves of the video mediastinoscope (21-23). This new approach was described to reduce the risk of vascular lesions.
Once the transcervical thoracoscopy is completed a small chest drain could be placed through the opening mediastinal pleura (Figure 12). The tube is connected to a suction system and if the air leak persists the tube could be externalized through the cervical incision, and fixed to the skin.
Comments
Transcervical VMT (1,2) was described by Deslauriers et al. in 1976. The absence of flexible endoscopes made that the procedure had not been fully applied. Many years later, the emergence of new endoscopes has allowed the revitalization of this technique (14,24).
Although this technique can offer different utilities we want to emphasize its role in staging in lung cancer and mesothelioma.
In lung cancer, a precise staging is crucial. In most patients with lung cancer, mediastinal staging is key to decide on the best therapeutic option. However, in those with an accompanying pleural effusion and negative thoracocentesis, its malignant nature must be confirmed or rule out, because if malignant nature is confirmed, tumour resection is not indicated.
We have different surgical techniques for staging lung cancers. At present, the improvement of endoscopic surgical techniques and their combination allow a more accurate staging with little surgical aggression to the patient (3).
VAMLA (5-8) gives us the possibility to perform a proper transcervical lymphadenectomy of the subcarinal and the right inferior paratracheal nodal stations and, thus, improving the accuracy of mediastinal staging compared to standard mediastinoscopy.
With mesothelioma the combination of VAMLA and transcervical thoracoscopy may increase the evidence on prognostic information. On the one hand, VAMLA informs us of nodal involvement (25) and, on the other hand, transcervical thoracoscopy allows the biopsy of material from the pleural surface helping to determine the subtype (epithelioid, biphasic and sarcomatoid). All this information is crucial in the decision-making of patients suitable for multimodality therapy (3).
From a single transcervical incision, VAMLA and video-thoracoscopy can be combined. With the 30º video-thoracoscope, the parietal and visceral pleura are visualized, as well as the inferior and lateral lung and pleural surface. In some cases, a flexible video-thoracoscope can be useful in order to visualise more of the chest cavity and improve the yield of the procedure in terms of obtaining tissue samples distant from the pleurotomy site (24). Through the valves of the video-mediastinoscope, it also is possible to take samples of pleural effusion introducing any suction system in the pleural cavity connected to a fluid container.
If malignancy is confirmed by frozen-section, a pleurodesis can be performed to avoid recurrence. Although many agents can be used, magnesium sulphate (talc) is effective, easy to be applied and cheap (26).
The access to the left pleural cavity is not so direct as on the right side because the supra-aortic vessels and the aortic arch have to be negotiated to reach the left mediastinal pleura. The route of the extended cervical mediastinoscopy, facilitates reaching the left mediastinal pleura to complete the diagnostic and/or therapeutic procedures (3).
Several relative or definitive contraindications of the technique are described. Mediastinal adhesions secondary to previous radiotherapy or surgery is the more common but it exists other contraindications like: pleural infection, mediastinal pleural invasion, posterior location of lung nodules, sever neck rigidity, large goitres, ascending aortic aneurism or atheromatosis of the aorta (3,10,14,27).
The most important difference with traditional thoracoscopy, is that you avoid a transthoracic approach. Avoidance of transthoracic ports probably decreases the risk of post-operative pain with no increase in surgical risk (28). Using a transcervical approach, we reduce the risk of wound recurrence due to its contamination with tumour cells in patients with malignant pleural mesothelioma (2,14).
Potential complications are described in Table 1 (2,7). Like in traditional mediastinoscopy, we have to be careful with the dissection of left paratracheal nodes to avoid the transient or permanent left recurrent laryngeal nerve palsy. Some series describe this complication after VAMLA in 3.2% of the patients (7).
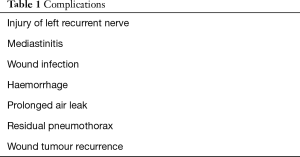
Full table
To reduce the risk of injury we recommend to visualize the nerve and avoidance of the electrocautery in close proximity to the nerve. Small bleedings near to the nerve should be controlled by temporary compression or clipping.
In conclusion, the developed in VATS has allowed the widespread application of video-assisted thoracoscopic surgical techniques. Regarding lung cancer and mesothelioma staging, it has allowed the combination of VAMLA and transcervical-thoracoscopy, improving the accuracy in staging of lung cancer and mesothelioma. By one incision we can answer many questions about diagnosis, staging and prognosis. For all these reasons, the combination of VAMLA and mediastino-thoracoscopy should be kept in mind for the described indications.
Acknowledgments
We would like to express our gratitude to Aitana Belda Camós and Josep Belda for drawing figures and to the rest of Thoracic Surgery Team, nurses and Anesthesiologists for allowing us to continue enjoying with our job.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors Marcin Zielinski and Qingdong Cao for the series “Mediastinoscopic Surgery” published in Mediastinum. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2019.05.02). The series “Mediastinoscopic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Deslauriers J, Beaulieu M, Dufour C, et al. Mediastinopleuroscopy: a new approach to the diagnosis of intrathoracic diseases. Ann Thorac Surg 1976;22:265-9. [Crossref] [PubMed]
- Chamberlain MH, Fareed K, Nakas A, et al. Video-assisted cervical thoracoscopy: a novel approach for diagnosis, staging and pleurodesis of malignant pleural mesothelioma. Eur J Cardiothorac Surg 2008;34:200-3. [Crossref] [PubMed]
- Dawson AG, Waller DA. Cervical mediastino-thoracoscopy. In: Zieliński M, Rami-Porta R. editors. The Transcervical Approach in Thoracic Surgery. Berlin Heidelberg: Springer-Verlag, 2014:45-51.
- Goldstraw P. editor. International Association for the Study of Lung Cancer Staging Handbook in Thoracic Oncology. Florida: Editorial Rx-Press, 2009.
- Hürtgen M, Friedel G, Toomes H, et al. Radical video-assisted mediastinoscopic lymphadenectomy (VAMLA) - technique and first results. Eur J Cardiothorac Surg 2002;21:348-51. [Crossref] [PubMed]
- Witte B, Hürtgen M. Video-assisted mediastinoscopic lymphadenectomy (VAMLA). J Thorac Oncol 2007;2:367-9. [Crossref] [PubMed]
- Call S, Obiols C, Rami-Porta R, et al. Video-assisted mediastinoscopic lymphadenectomy for staging non-small cell lung cancer. Ann Thorac Surg 2016;101:1326-33. [Crossref] [PubMed]
- Witte B, Huertgen M. Video-assisted mediastinoscopic lymphadenectomy. Multimed Man Cardiothorac Surg 2007. Doi: mmcts.2006.002576.
- Rusch VW, Asamura H, Watanabe H, et al. The IASLC lung cancer staging project. A proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4:568-77.
- Call S, Rami Porta R, Serra Mitjans M, et al. Extended cervical mediastinoscopy in the staging of bronchogenic carcinoma of the left lung. Eur J Cardiothorac Surg 2008;34:1081-4. [Crossref] [PubMed]
- Lopez L, Varela A, Freixinet J, et al. Extended cervical mediastinoscopy: prospective study of fifty cases. Ann Thorac Surg 1994;57:555-7; discussion 557-8. [Crossref] [PubMed]
- Freixinet Gilart J, Gamez P, Rodriguez de Castro P, et al. Extended cervical mediastinoscopy in the staging of bronchogenic carcinoma. Ann Thorac Surg 2000;70:1641-3. [Crossref] [PubMed]
- Obiols C, Call S, Rami-Porta R, et al. Utility of the transcervical approach in bilateral synchronous lung cancer. Asian Cardiovasc Thorac Ann 2015;23:991-4. [Crossref] [PubMed]
- Fowkes L, Lau KKW, Shah N, et al. A cervical approach to investigating pleural disease. Ann Thorac Surg 2009;88:315-7. [Crossref] [PubMed]
- De Leyn P, Dooms C, Kuzdal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;45:787-98. [Crossref] [PubMed]
- Trujillo-Reyes JC, Martínez-Téllez E. Subcarinal lymphadenectomy. Asvide 2019;6:148. Available online: http://www.asvide.com/article/view/32079
- Trujillo-Reyes JC, Martínez-Téllez E. Right paratracheal lymphadenectomy. Asvide 2019;6:149. Available online: http://www.asvide.com/article/view/32080
- Trujillo-Reyes JC, Martínez-Téllez E. Left paratracheal lymphadenectomy. Asvide 2019;6:150. Available online: http://www.asvide.com/article/view/32081
- Trujillo-Reyes JC, Martínez-Téllez E. Right transcervical thoracoscopy. Asvide 2019;6:151. Available online: http://www.asvide.com/article/view/32082
- Ginsberg RJ, Rice TW, Goldberg M, et al. Extended cervical mediastinoscopy. A single staging procedure for bronchogenic carcinoma of the left upper lobe. J Thorac Cardiovasc Surg 1987;94:673-8. [PubMed]
- Assouad J, Fénane H, Masmoudi H, et al. Flexible endoscope in thoracic surgery: CITES or cVATS? Rev Pneumol Clin 2013;69:294-7. [Crossref] [PubMed]
- Masmoudi H, Karsenti A, Giol M, et al. Cervical and retrosternal approach to the left thoracic cavity using a flexible endoscope. Interact Cardiovasc Thorac Surg 2014;18:784-8. [Crossref] [PubMed]
- Assouad J, Steltzlen C, Masmoudi H, et al. Cervical incision thoracic endoscopic surgery: a minimally invasive endoscopic approach in thoracic surgery. Interact Cardiovasc Thorac Surg 2010;10:967-70. [Crossref] [PubMed]
- Liberman M, Khereba M, Goudie E, et al. Cervical video- assisted thoracoscopic surgery using a flexible endoscope for bilateral thoracoscopy. Ann Thorac Surg 2012;93:1321-3. [Crossref] [PubMed]
- Rusch VW, Venkatraman E. The importance of surgical staging in the treatment of malignant pleural mesothelioma. J Thorac Cardiovasc Surg 1996;111:815-25; discussion 825-6. [Crossref] [PubMed]
- Lee YC, Baumann MH, Maskell NA, et al. Pleurodesis practice for malignant pleural effusions in five English-speaking countries, survey of pulmonologists. Chest 2003;124:2229-38. [Crossref] [PubMed]
- Trujillo-Reyes JC, Martínez-Téllez E, Rami-Porta R, et al. Combination video-assisted mediastinoscopic lymphadenectomy and transcervical thoracoscopy. Multimed Man Cardiothorac Surg 2018; [Crossref] [PubMed]
- Zieliński M, Pankowski J, Hauer L, et al. The right upper lobe pulmonary resection performed through the transcervical approach. Eur J Cardiothorac Surg 2007;32:766-9. [Crossref] [PubMed]
Cite this article as: Trujillo-Reyes JC, Martínez-Téllez E. Video-assisted mediastinoscopic lymphadenectomy combined with transcervical thoracoscopy. Mediastinum 2019;3:21.






