
Mediastinal lymph node staging for lung cancer
Introduction
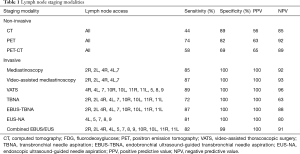
The presence or absence of lymph node metastasis in lung carcinoma has a significant effect on the treatment policy and prognosis. Recent advances in medical technology has helped establish several new methods for diagnosis—fluorodeoxyglucose positron emission tomography (FDG-PET), PET-computed tomography (CT), transbronchial needle aspiration (TBNA), endobronchial ultrasound-guided TBNA (EBUS-TBNA), convex type EBUS-TBNA, endoscopic ultrasound-guided needle aspiration (EUS-NA), mediastinoscopy (MED), video-assisted MED (VAM), and video-assisted thoracoscopic surgery (VATS). The combined use of non-invasive and invasive methods for the diagnosis of lymph node metastasis is challenging and the features of each method must be carefully considered before choosing them (Table 1).
Full table
Non-invasive methods (diagnostic imaging)
Non-invasive diagnostic imaging such as CT, FDG-PET, and PET-CT, can detect all lymph nodes in the chest, however positive predictive values (PPVs) are not high in spite of a relatively high negative predictive value. Presently, there is no substitute for histological examination, and invasive methods are required only for the final diagnosis
CT
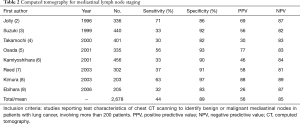
Various criteria for the diagnosis of mediastinal lymph node metastasis by CT have been proposed such as the product of the major and minor axis, size of the transition by station, and change of the standard by tissue type (1). Since there is presently no consensus, lymph nodes measuring more than 1 cm at the minor axis are considered as metastatic. Several reports have used this method to confirm metastasis in case of a surgical adaptation; mean sensitivity and specificity are 44% and 89% (Table 2).
Full table
FDG-PET/FDG-PE-CT
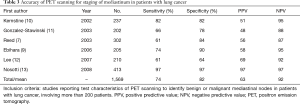
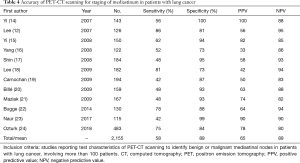
FDG-PET use has been ubiquitous due to the development of the delivery system. It was initially considered as a substitute for cytology or tissue sampling for the diagnosis of cancer, but it should be used with care as false positives and false negatives are seen occasionally (Table 3), and careful evaluation is necessary for the diagnosis of mediastinal lymph nodes. However, a good quality image, and fusion PET-CT provides accurate information for diagnosis (Table 4). An FDG is known to accumulate in lymph nodes in non-malignant conditions such as inflammation and the results can be pseudo positive as the specificity or negative predictive values are relatively low. The Z0050 trial (7) which analyzed the use of PET for staging in 303 cases of non-small cell lung carcinoma with surgical adaptation revealed an N1 detection rate of 13% vs. 42%, N2 and N3 detection of 32% vs. 58%, and sensitivity of 37% vs. 61%, by CT and PET scans respectively. This makes it possible to prevent unnecessary thoracotomies; however, a definite diagnosis is still necessary for confirmatory findings.
Full table
Full table
Invasive methods (cytological-pathological diagnosis)
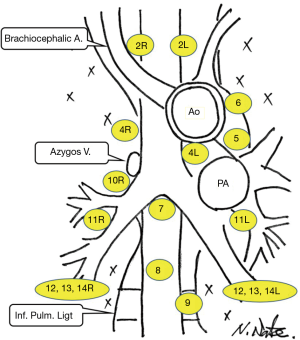
It is necessary to perform an invasive procedure such as MED, VAM, VATS, TBNA, EBUS-TBNA, or EUS-NA (sensitivity of the needle biopsy is lower in the case of N0) even after PET scans show positive or negative lymph nodes. The most appropriate method is chosen according to the surgeon’s skill, experience, and lymph node position (Figure 1).
MED and VATS
Traditionally, lymph nodes sampling is carried under direct visualization, but currently it is done by viewing an image on the video monitor and is performed with more safety. Additionally, the accuracy of MED is similar to MED and VAM (Table 5). A report on MED in 202 cases after a PET scan (11) revealed that only 29 cases were PET-positive, while 65 cases were positive in MED; N2 and N3 stages were observed in 16 out of 137 PET negative cases. MED is considered to be a standard procedure by some for the diagnosis of mediastinal lymph nodes. VATS has been used to assess aorto-pulmonary window lymph nodes (level 5) and paraaortic lymph nodes (level 6). The overall results of this technique are summarized in Table 6. Specific results for stations 5 and 6 have not been reported but are likely to be better because these are easier to access than other mediastinal node stations. In specific cases, a combination of VAM and VATS is performed for the management of lung cancer (39).
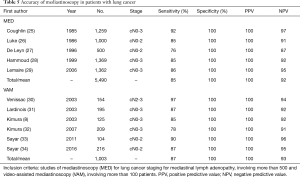
Full table

Full table
TBNA
Although TBNA has been used for some time, the rate of diagnosis is greatly affected by the experience of the examiner and is no longer used as a standard diagnostic tool. The results of studies on TBNA containing more than 100 cases is shown in Table 7, and reveals that mean specificity, sensitivity, PPV, and negative predictive values were 72%, 100%, 100%, and 63%, respectively.
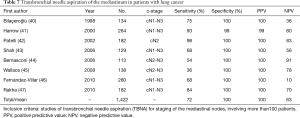
Full table
EBUS-TBNA/EUS-NA
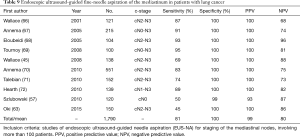
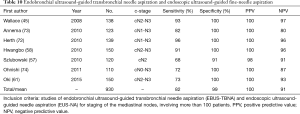
The method of identifying the position of lymph nodes using ultrasound to increase the accuracy of the lymph node metastasis has progressed. The combined results of lymph node metastasis by EBUS-TBNA from various studies are summarized in Table 8.
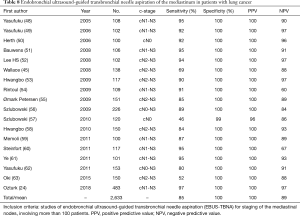
Full table
The convex-operated ultrasonic bronchoscopic needle biopsy method (Convex probe EBUS-TBNA) has recently emerged as a popular technique. Yasufuku et al. was the first to perform an EBUS-TBNA using a convex type model (64). A total of 70 patients with a confirmed or suspected malignant tumor, with lymph nodes of more than 1 cm on CT (mediastinal lymph nodes 58 cases, hilar lymph nodes 12 cases) were analyzed in real-time. According to the report, 68 positive cases were identified from the patients with lymph nodes, and two cases were found to be negative. Forty-five cases were found to be malignant and 25 were benign. The test results showed that sensitivity, specificity, and accuracy were 95.7%, 100%, and 97.1%, respectively. The patients had good results, and no complications were reported. In another study, Yasufuku et al. compared CT, PET, and EBUS-TBNA in patients with lung cancer or suspected surgical adaptation in published reports and reported that their respective sensitivities were 76.9%, 80.0%, 92.3%; specificities were 55.3%, 70.1%, 100%; and accuracies were 60.8%, 72.5%, 98.0%. EBUS-TBNA was found to have excellent results (65).
The CT is inaccurate and so is the PET, although it increased the possibility of different diagnoses. The TBNA is a blind procedure, and the CT-guided cytology is more restrictive than the conventional ultrasound guided cytology, and the standard MED is also restricted and invasive. Although a TBNA cannot reach levels 5, 6, 8, 9 of lymph nodes, it is possible to access levels 10 and 11, and the total mediastinum can be reached when combined with EUS-NA. In addition, if the MED and EBUS-TBNA are compared, the EBUS-TBNA may reduce the necessity of a MED without complications; however, it is necessary to assess the possibility of micro metastases by EBUS-TBNA.
An EUS-NA is a transesophageal ultrasound endoscope, which can access parts unreachable by mediastinoscope and is more accurate than a PET or CT; its PPV is particularly good (Table 9). An EUS-NA and an EBUS-TBNA are complementary technologies and can be adapted to be used together (Table 10).
Full table
Full table
Conclusions
Although techniques for mediastinal lymph node diagnosis should be chosen depending on the experience and skill of the surgeon, the relatively minimally invasive EBUS-TBNA is preferred to obtain a histological diagnosis. However, more advanced technologies to match the pathological diagnosis by PET imaging are expected in the future.
Acknowledgments
We would like to thank Editage (
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2019.07.04). NS serves as an unpaid editorial board member of Mediastinum from Feb 2018 to Jan 2020. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ikezoe J, Kadowaki K, Morimoto S, et al. Mediastinal lymph node metastases from nonsmall cell bronchogenic carcinoma: reevaluation with CT. J Comput Assist Tomogr 1990;14:340-4. [Crossref] [PubMed]
- Jolly PC, Hutchinson CH, Detterbeck F, et al. Routine computed tomographic scans, selective mediastinoscopy, and other factors in evaluation of lung cancer. J Thorac Cardiovasc Surg 1991;102:266-70. [PubMed]
- Suzuki K, Nagai K, Yoshida J, et al. Clinical predictors of N2 disease in the setting of a negative computed tomographic scan in patients with lung cancer. J Thorac Cardiovasc Surg 1999;117:593-8. [Crossref] [PubMed]
- Takamochi K, Nagai K, Yoshida J, et al. The role of computed tomographic scanning in diagnosing mediastinal node involvement in non-small cell lung cancer. J Thorac Cardiovasc Surg 2000;119:1135-40. [Crossref] [PubMed]
- Osada H, Kojima K, Tsukada H, et al. Cost-effectiveness associated with the diagnosis and staging of non-small-cell lung cancer. Jpn J Thorac Cardiovasc Surg 2001;49:1-10. [Crossref] [PubMed]
- Kamiyoshihara M, Kawashima O, Ishikawa S, et al. Mediastinal lymph node evaluation by computed tomographic scan in lung cancer. J Cardiovasc Surg (Torino) 2001;42:119-24. [PubMed]
- Reed CE, Harpole DH, Posther KE, et al. American College of Surgeons Oncology Group Z0050 trial. Results of the American College of Surgeons Oncology Group Z0050 trial: the utility of positron emission tomography in staging potentially operable non-small cell lung cancer. J Thorac Cardiovasc Surg 2003;126:1943-51. [Crossref] [PubMed]
- Kimura H, Iwai N, Ando S, et al. A prospective study of indications for mediastinoscopy in lung cancer with CT findings, tumor size, and tumor markers. Ann Thorac Surg 2003;75:1734-9. [Crossref] [PubMed]
- Ebihara A, Nomori H, Watanabe K, et al. Characteristics of advantages of positron emission tomography over computed tomography for N-staging in lung cancer patients. Jpn J Clin Oncol 2006;36:694-8. [Crossref] [PubMed]
- Kernstine KH, McLaughlin KA, Menda Y, et al. Can FDG PET reduce the need for mediastinoscopy in potentially resectable nonsmall cell lung cancer? Ann Thorac Surg 2002;73:394-401. [Crossref] [PubMed]
- Gonzalez-Stawinski GV, Lemaire A, Merchant F, et al. A comparative analysis of positron emission tomography and mediastinoscopy in staging non-small cell lung cancer. J Thorac Cardiovasc Surg 2003;126:1900-5. [Crossref] [PubMed]
- Lee BE, von Haag D, Lown T, et al. Advances in positron emission tomography technology have increased the need for surgical staging in non-small cell lung cancer. J Thorac Cardiovasc Surg 2007;133:746-52. [Crossref] [PubMed]
- Nosotti M, Castellani M, Longari V, et al. Staging non-small lung cancer with positron emission tomography: diagnostic value, impact on patient management, and cost-effectiveness. Int Surg 2008;93:278-83. [PubMed]
- Yi CA, Lee KS, Kim BT, et al. Efficacy of helical dynamic CT versus integrated PET/CT for detection of mediastinal nodal metastasis in non-small cell lung cancer. AJR Am J Roentgenol 2007;188:318-25. [Crossref] [PubMed]
- Yi CA, Shin KM, Lee KS, et al. Non-small cell lung cancer staging: efficacy comparison of integrated PET/CT versus 3.0-T whole-body MR imaging. Radiology 2008;248:632-42. [Crossref] [PubMed]
- Yang W, Fu Z, Yu J, et al. Value of PET/CT versus enhanced CT for locoregional lymph nodes in non-small cell lung cancer. Lung Cancer 2008;61:35-43. [Crossref] [PubMed]
- Shin KM, Lee KS, Shim YM, et al. FDG PET/CT and mediastinal nodal metastasis detection in stage T1 non-small cell lung cancer: prognostic implications. Korean J Radiol 2008;9:481-9. [Crossref] [PubMed]
- Lee JW, Kim BS, Lee DS, et al. 18F-FDG PET/CT in mediastinal lymph node staging of non-small-cell lung cancer in a tuberculosis-endemic country: consideration of lymph node calcification and distribution pattern to improve specificity. Eur J Nucl Med Mol Imaging 2009;36:1794-802. [Crossref] [PubMed]
- Carnochan FM, Walker WS. Positron emission tomography may underestimate the extent of thoracic disease in lung cancer patients. Eur J Cardiothorac Surg 2009;35:781-4. [Crossref] [PubMed]
- Billé A, Pelosi E, Skanjeti A, et al. Preoperative intrathoracic lymph node staging in patients with non-small-cell lung cancer: accuracy of integrated positron emission tomography and computed tomography. Eur J Cardiothorac Surg 2009;36:440-5. [Crossref] [PubMed]
- Maziak DE, Darling GE, Inculet RI, et al. Positron emission tomography in staging early lung cancer: a randomized trial. Ann Intern Med 2009;151:221-8, W-48.
- Bugge AS, Naalsund A, Johnsrud K, et al. PET-CT in the assessment of lung cancer at Rikshospitalet from 2007-2011. Tidsskr Nor Laegeforen 2014;134:938-44. [Crossref] [PubMed]
- Naur TMH, Konge L, Clementsen PF. Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration for Staging of Patients with Non-Small Cell Lung Cancer without Mediastinal Involvement at Positron Emission Tomography-Computed Tomography. Respiration 2017;94:279-84. [Crossref] [PubMed]
- Ozturk A, Gullu YT. Excellence in non-small cell lung cancer staging by endobronchial-TBNA: Comparison with PET-CT and surgery. Minim Invasive Ther Allied Technol 2019;28:213-9. [Crossref] [PubMed]
- Coughlin M, Deslauriers J, Beaulieu M, et al. Role of mediastinoscopy in pretreatment staging of patients with primary lung cancer. Ann Thorac Surg 1985;40:556-60. [Crossref] [PubMed]
- Luke WP, Pearson FG, Todd TR, et al. Prospective evaluation of mediastinoscopy for assessment of carcinoma of the lung. J Thorac Cardiovasc Surg 1986;91:53-6. [PubMed]
- De Leyn P, Schoonooghe P, Deneffe G, et al. Surgery for non-small cell lung cancer with unsuspected metastasis to ipsilateral mediastinal or subcarinal nodes (N2 disease). Eur J Cardiothorac Surg 1996;10:649-54. [Crossref] [PubMed]
- Hammoud ZT, Anderson RC, Meyers BF, et al. The current role of mediastinoscopy in the evaluation of thoracic disease. J Thorac Cardiovasc Surg 1999;118:894-9. [Crossref] [PubMed]
- Lemaire A, Nikolic I, Petersen T, et al. Nine-year single center experience with cervical mediastinoscopy: complications and false negative rate. Ann Thorac Surg 2006;82:1185-9; discussion 1189-90. [Crossref] [PubMed]
- Venissac N, Alifano M, Mouroux J. Video-assisted mediastinoscopy: experience from 240 consecutive cases. Ann Thorac Surg 2003;76:208-12. [Crossref] [PubMed]
- Lardinois D, Schallberger A, Betticher D, et al. Postinduction video-mediastinoscopy is as accurate and safe as video-mediastinoscopy in patients without pretreatment for potentially operable non-small cell lung cancer. Ann Thorac Surg 2003;75:1102-6. [Crossref] [PubMed]
- Kimura H, Yasufuku K, Ando S, et al. Indications for mediastinoscopy and comparison of lymph node dissections in candidates for lung cancer surgery. Lung Cancer 2007;56:349-55. [Crossref] [PubMed]
- Sayar A, Citak N, Metin M, et al. Comparison of video assisted mediastinoscopy and video-assisted mediastinoscopic lymphadenectomy for lung cancer. Gen Thorac Cardiovasc Surg 2011;59:793-8. [Crossref] [PubMed]
- Sayar A, Çitak N, Büyükkale S, et al. The incidence of hoarseness after mediastinoscopy and outcome of video-assisted versus conventional mediastinoscopy in lung cancer staging. Acta Chir Belg 2016;116:23-9. [Crossref] [PubMed]
- Eggeling S, Martin T, Böttger J, et al. Invasive staging of non-small cell lung cancer--a prospective study. Eur J Cardiothorac Surg 2002;22:679-84. [Crossref] [PubMed]
- Massone PP, Lequaglie C, Magnani B, et al. The real impact and usefulness of video-assisted thoracoscopic surgery in the diagnosis and therapy of clinical lymphadenopathies of the mediastinum. Ann Surg Oncol 2003;10:1197-202. [Crossref] [PubMed]
- Sebastián-Quetglás F, Molins L, Baldó X, et al. Clinical value of video-assisted thoracoscopy for preoperative staging of non-small cell lung cancer. A prospective study of 105 patients. Lung Cancer 2003;42:297-301. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Eloubeidi MA. Accessing the aortopulmonary window (#5) and the paraaortic (#6) lymph nodes in patients with non-small cell lung cancer. Ann Thorac Surg 2007;84:940-5. [Crossref] [PubMed]
- Mouroux J, Venissac N, Alifano M. Combined video-assisted mediastinoscopy and video-assisted thoracoscopy in the management of lung cancer. Ann Thorac Surg 2001;72:1698-704. [Crossref] [PubMed]
- Bilaçeroğlu S, Cağiotariotaciota U, Günel O, et al. Comparison of rigid and flexible transbronchial needle aspiration in the staging of bronchogenic carcinoma. Respiration 1998;65:441-9. [Crossref] [PubMed]
- Harrow EM, Abi-Saleh W, Blum J, et al. The utility of trans bronchial needle aspiration in the staging of bronchogenic carcinoma. Am J Respir Crit Care Med 2000;161:601-7. [Crossref] [PubMed]
- Patelli M, Lazzari Agli L, Poletti V, et al. Role of fiberscopic transbronchial needle aspiration in the staging of N2 disease due to non-small cell lung cancer. Ann Thorac Surg 2002;73:407-11. [Crossref] [PubMed]
- Shah P L, Singh S, Bower M, et al. The role of transbronchial fi ne needle aspiration in an integrated care pathway for the assessment of patients with suspected lung cancer. J Thorac Oncol 2006;1:324-7. [Crossref] [PubMed]
- Bernasconi M, Chhajed PN, Gambazzi F, et al. Combined transbronchial needle aspiration and positron emission tomography for mediastinal staging of NSCLC. Eur Respir J 2006;27:889-94. [Crossref] [PubMed]
- Wallace MB, Pascual JM, Raimondo M, et al. Minimally invasive endoscopic staging of suspected lung cancer. JAMA 2008;299:540-6. [Crossref] [PubMed]
- Fernández-Villar A, Botana M, Leiro V, et al. Validity and reliability of transbronchial needle aspiration for diagnosing mediastinal adenopathies. BMC Pulm Med 2010;10:24. [Crossref] [PubMed]
- Rakha EA, Naik V, Chaudry Z, et al. Cytological assessment of conventional transbronchial fine needle aspiration of lymph nodes. Cytopathology 2010;21:27-34. [Crossref] [PubMed]
- Yasufuku K, Chiyo M, Koh E, et al. Endobronchial ultrasound guided transbronchial needle aspiration for staging oflung cancer. Lung Cancer 2005;50:347-54. [Crossref] [PubMed]
- Yasufuku K, Nakajima T, Motoori K, et al. Comparison of endobronchial ultrasound, positron emission tomography, and CT for lymph node staging of lung cancer. Chest 2006;130:710-8. [Crossref] [PubMed]
- Herth FJ, Ernst A, Eberhardt R, et al. Endobronchial ultrasound-guided transbronchial needle aspiration of lymph nodes in the radiologically normal mediastinum. Eur Respir J 2006;28:910-4. [Crossref] [PubMed]
- Bauwens O, Dusart M, Pierard P, et al. Endobronchial ultrasound and value of PET for prediction of pathological results of mediastinal hot spots in lung cancer patients. Lung Cancer 2008;61:356-61. [Crossref] [PubMed]
- Lee BE, Kletsman E, Rutledge JR, et al. Utility of endobronchial ultrasound-guided mediastinal lymph node biopsy in patients with non-small cell lung cancer. J Thorac Cardiovasc Surg 2012;143:585-90. [Crossref] [PubMed]
- Hwangbo B, Kim SK, Lee HS, et al. Application of endobronchial ultrasound-guided transbronchial needle aspiration following integrated PET/CT in mediastinal staging of potentially operable non-small cell lung cancer. Chest 2009;135:1280-7. [Crossref] [PubMed]
- Rintoul RC, Tournoy KG, El Daly H, et al. EBUS-TBNA for the clarification of PET positive intra-thoracic lymph nodes-an international multi-center experience. J Thorac Oncol 2009;4:44-8. [Crossref] [PubMed]
- Ømark Petersen H, Eckardt J, Hakami A, et al. The value of mediastinal staging with endobronchial ultrasound-guided transbronchial needle aspiration in patients with lung cancer. Eur J Cardiothorac Surg 2009;36:465-8. [Crossref] [PubMed]
- Szlubowski A, Kuzdzał J, Kołodziej M, et al. Endobronchial ultrasound-guided needle aspiration in the non-small cell lung cancer staging. Eur J Cardiothorac Surg 2009;35:332-5; discussion 335-6. [Crossref] [PubMed]
- Szlubowski A, Zieliński M, Soja J, et al. A combined approach of endobronchial and endoscopic ultrasound-guided needle aspiration in the radiologically normal mediastinum in non-small-cell lung cancer staging--a prospective trial. Eur J Cardiothorac Surg 2010;37:1175-9. [Crossref] [PubMed]
- Hwangbo B, Lee GK, Lee HS, et al. Transbronchial and transesophageal fine-needle aspiration using an ultrasound bronchoscope in mediastinal staging of potentially operable lung cancer. Chest 2010;138:795-802. [Crossref] [PubMed]
- Wang Memoli JS, El-Bayoumi E, Pastis NJ, et al. Using endobronchial ultrasound features to predict lymph node metastasis in patients with lung cancer. Chest 2011;140:1550-6. [Crossref] [PubMed]
- Steinfort DP, Hew MJ, Irving LB. Bronchoscopic evaluation of the mediastinum using endobronchial ultrasound: a description of the first 216 cases carried out at an Australian tertiary hospital. Intern Med J 2011;41:815-24. [Crossref] [PubMed]
- Ye T, Hu H, Luo X, et al. The role of endobronchial ultrasound guided transbronchial needle aspiration (EBUS-TBNA) for qualitative diagnosis of mediastinal and hilar lymphadenopathy: a prospective analysis. BMC Cancer 2011;11:100. [Crossref] [PubMed]
- Yasufuku K, Pierre A, Darling G, et al. A prospective controlled trial of endobronchial ultrasound-guided transbronchial needle aspiration compared with mediastinoscopy for mediastinal lymph node staging of lung cancer. J Thorac Cardiovasc Surg 2011;142:1393-400.e1. [Crossref] [PubMed]
- Oki M, Saka H, Ando M, et al. Endoscopic ultrasound-guided fine needle aspiration and endobronchial ultrasound-guided transbronchial needle aspiration: Are two better than one in mediastinal staging of non-small cell lung cancer? J Thorac Cardiovasc Surg 2014;148:1169-77. [Crossref] [PubMed]
- Yasufuku K, Chiyo M, Sekine Y, et al. Real-time endobronchial ultrasound guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest 2004;126:122-8. [Crossref] [PubMed]
- Yasufuku K, Nakajima T, Chiyo M, et al. Endobronchial ultrasonography: current status and future directions. J Thorac Oncol 2007;2:970-9. [Crossref] [PubMed]
- Wallace MB, Silvestri G, Sahai AV, et al. Endoscopic ultrasound-guided fi ne needle aspiration for staging patients with carcinoma of the lung. Ann Thorac Surg 2001;72:1861-7. [Crossref] [PubMed]
- Annema JT, Versteegh MI, Veseli M, et al. Endoscopic ultrasound-guided fi ne-needle aspiration in the diagnosis and staging of lung cancer and its impact on surgical staging. J Clin Oncol 2005;23:8357-61. [Crossref] [PubMed]
- Eloubeidi MA, Cerfolio RJ, Chen VK, et al. Endoscopic ultrasound-guided fi ne needle aspiration of mediastinal lymph node in patients with suspected lung cancer after positron emission tomography and computed tomography scans. Ann Thorac Surg 2005;79:263-8. [Crossref] [PubMed]
- Tournoy KG, Ryck FD, Vanwalleghem L, et al. The yield of endoscopic ultrasound in lung cancer staging: does lymph node size matter? J Thorac Oncol 2008;3:245-9. [Crossref] [PubMed]
- Annema JT, Bohoslavsky R, Burgers S, et al. Implementation of endoscopic ultrasound for lung cancer staging. Gastrointest Endosc 2010;71:64-70. [Crossref] [PubMed]
- Talebian M, von Bartheld MB, Braun J, et al. EUS-FNA in the preoperative staging of non-small cell lung cancer. Lung Cancer 2010;69:60-5. [Crossref] [PubMed]
- Herth FJ, Krasnik M, Kahn N, et al. Combined endoscopic-endobronchial ultrasound-guided fine-needle aspiration of mediastinal lymph nodes through a single bronchoscope in 150 patients with suspected lung cancer. Chest 2010;138:790-4. [Crossref] [PubMed]
- Annema JT, van Meerbeeck JP, Rintoul RC, et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer: a randomized trial. JAMA 2010;304:2245-52. [Crossref] [PubMed]
- Ohnishi R, Yasuda I, Kato T, et al. Combined endobronchial and endoscopic ultrasound-guided fi ne needle aspiration for mediastinal nodal staging of lung cancer. Endoscopy 2011;43:1082-9. [Crossref] [PubMed]
Cite this article as: Sawabata N. Mediastinal lymph node staging for lung cancer. Mediastinum 2019;3:33.


