A case report of a giant middle mediastinal leiomyosarcoma
Introduction
Leiomyosarcomas account for 5% to 10% of soft tissue sarcomas (1). Most common sites for primary leiomyosarcomas are the extremity, retroperitoneum and uterus. But they can theoretically arise at any anatomical sites. Most mediastinal tumors arise from the anterior mediastinal compartment (2). Tumors of the middle compartment are very rare, with a prevalence of 0.1% in a healthy population who underwent check-up related chest computed tomography (CT) (2). Leiomyosarcomas of the mediastinum are exceptionally rare and most often arise from the middle-posterior mediastinum, involving mediastinal structures such as oesophagus, heart or great vessels (3,4). Less than 40 cases were described in small series and case reports (3).
Here we report the rare case of a patient with a giant middle mediastinal leiomyosarcoma treated surgically, which did not show any involvement of neighbouring structures. We present the following case in accordance with the CARE reporting checklist (available at https://med.amegroups.com/article/view/10.21037/med-21-44/rc). Patient specific information was de-identified.
Case presentation
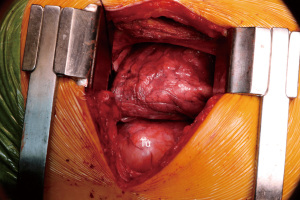
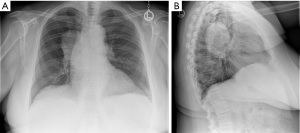
A 70-year-old obese female with a history of chronic obstructive pulmonary disease (COPD) and atrial fibrillation presented to her general practitioner with dry cough and increasing shortness of breath for the last six months. She had no previous surgical history. No relevant findings on clinical examination were noted. Chest X-ray in both projections showed a mediastinal mass (Figure 1A,1B). The patient was transferred to our unit for additional work-up. Chest computed tomography (CT) confirmed a giant middle mediastinal tumor measuring up to 11 cm in its largest diameter (Figure 2). Bronchoscopy and oesophagoscopy did show extrinsic compression of the tracheal carina and oesophagus without endoluminal tumor. Pathological tumor sampling was performed with endobronchial ultrasound-fine-needle aspiration (EBUS-FNA). Spindle cell complexes were noted on microscopy. Immunohistochemical evaluation of tumor was negative for CD34, CD56, S100, STAT6 and synaptophysin. Tumor cells were positive for actin, caldesmon and desmin. Ki-67 was 20%. Immunohistochemical profile was compatible with a myogenous tumor with moderate proliferation rate, most likely leiomyosarcoma. Staging was completed with positron emission tomography fused with computed tomography (PET/CT), which did not show distant metastases. Preoperative magnetic resonance imaging (MRI) excludes oesophageal infiltration. The case was presented in our multidisciplinary sarcoma tumor board and upfront surgery was decided due to patient’s age and high symptom burden.

A muscle sparing fifth intercostal space posterolateral thoracotomy on the right was performed and the chest was entered. The tumor was located in the middle mediastinum (Figure 3). The pulmonary ligament was divided and the mediastinal pleura opened. The tumor was sharply dissected and mobilized from all surrounding structures, namely the lung, airways, oesophagus and spine. None of these structures were infiltrated by the tumor. The tumor was extracted from the chest. Paratracheal, subcarinal and hilar lymph node dissection was performed. Postoperative hospital stay was uneventful. The patient was discharged on postoperative day 6.
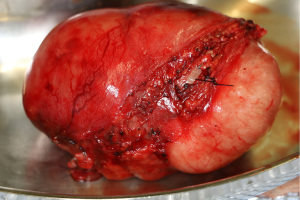
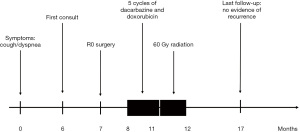
Macroscopic view of the resected specimen is depicted in Figure 4. Histopathological microscopic examination confirmed a conventional G2 leiomyosarcoma. MDM2 molecular testing was not performed since intimal sarcoma was intraoperatively excluded. Indeed, the tumor arose separately from any obvious vessels. Tumor margins and all 37 mediastinal lymph nodes were free of tumor (R0). The patient was presented to our multidisciplinary sarcoma tumor board and adjuvant chemoradiation was advised. She underwent 5 cycles of dacarbazine and doxorubicin followed by 60 Gy. Ten months after surgery the patient is well and does not show evidence of recurrence on CT imaging. A timeline picture of Historical and current information from this episode of care is depicted in Figure 5.
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and the accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Primary mediastinal sarcomas are rare cancers, accounting approximately for 1% of all soft tissue sarcomas (5). Due to their location and size at diagnosis, fewer than half (48.9%) of patients with mediastinal sarcoma underwent surgery, based on the analysis of the National Cancer Database including 976 patients (6). However, whenever feasible, complete resection should be attempted. In 477 patients who underwent surgery, overall survival was significantly better for patients with microscopically complete (R0) resection (30.1% vs. 18.9%, P=0.002) (6).
Preoperative pathologic diagnosis of mediastinal tumors is important since it will guide further multimodality treatment and surgical planning. Depending on tumor size and location, mediastinal tumors are usually preoperatively diagnosed with EBUS-FNA, EUS-FNA, percutaneous CT-guided biopsy, mediastinoscopy, mediastinotomy and VATS. The use of FNA cytology for the diagnosis of mediastinal sarcoma is debated and uncommonly employed. However, in our case, leiomyosarcoma diagnosis could be successfully done with FNA cytology, where cell morphology was paired with ancillary immunohistochemical staining and molecular methods, as mentioned elsewhere (7).
Primary mediastinal leiomyosarcoma is a rarity, encountered in adult patients from 28 to 88 (3). It accounts for 10.4% to 14.3% of all mediastinal sarcomas (6,8,9). Surgical strategy depends on leiomyosarcoma origin, size, location and growth pattern. Mediastinal leiomyosarcomas may develop from the heart (10), oesophagus (11) or great vessels (12,13). In other cases, major structures such as the inferior vena cava may be entrapped by the leiomyosarcoma without infiltration (14). Resection implies en-bloc resection of the involved structure. In our case, leiomyosarcoma presented as a mass compressing neighbouring structures without encasement or infiltration. Ten similar patients were described in an early case series (15). Resection consisted in tumor removal, leaving neighbouring structures unresected as in our report (15).
The origin of such leiomyosarcoma is controversial. An origin from small vessels within mediastinal soft tissue was hypothesised, while others speculated an origin from heterotopic smooth muscle displaced during embryogenesis or from an oesophageal tumor that detached from its wall during its growth (15-17).
No meaningful data on overall survival for primary mediastinal leiomyosarcoma were reported since data are issued from case reports or small series of two to three patients (8,9). In the largest series of primary mediastinal sarcomas, 101 patients with leiomyosarcoma were reported (6). Unfortunately, overall survival rate for leiomyosarcoma subgroup was not reported. But results of cox proportional hazards model showed a significant better survival for leiomyosarcoma histology compared to the reference and worst survival-related histology of hemangiosarcoma [hazard ratio (HR) 0.48, 95% confidence interval (CI): 0.35–0.66] (6).
In conclusion, leiomyosarcoma is a rare tumor that may arise from the middle mediastinum as a giant tumor. Preoperative imaging and diagnosis are key in planning surgical treatment and multimodality therapy as for other mediastinal tumors. Future case descriptions are encouraged to optimize management and outcome of primary mediastinal leiomyosarcomas.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ryuichi Waseda and Pietro Bertoglio) for the series “Management of Giant Mediastinal Tumors” published in Mediastinum. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://med.amegroups.com/article/view/10.21037/med-21-44/rc
Peer Review File: Available at https://med.amegroups.com/article/view/10.21037/med-21-44/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-21-44/coif). The series “Management of Giant Mediastinal Tumors” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects for the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Penel N, Italiano A, Isambert N, et al. Factors affecting the outcome of patients with metastatic leiomyosarcoma treated with doxorubicin-containing chemotherapy. Ann Oncol 2010;21:1361-5. [Crossref] [PubMed]
- Kasuga I, Maezawa H, Gamo S, et al. Prevalence of Mediastinal Tumors Using Low-Dose Spiral Computed Tomography in Healthy Population. J Thorac Oncol 2018;13:S605. [Crossref]
- den Bakker MA, Marx A, Mukai K, et al. Mesenchymal tumours of the mediastinum--part II. Virchows Arch 2015;467:501-17. [Crossref] [PubMed]
- Ishikawa A, Kuraoka K, Zaitsu J, et al. Anterior Mediastinal Leiomyosarcoma: A Case Report and Literature Review. Case Rep Oncol 2021;14:101-6. [Crossref] [PubMed]
- Burt M, Ihde JK, Hajdu SI, et al. Primary sarcomas of the mediastinum: results of therapy. J Thorac Cardiovasc Surg 1998;115:671-80. [Crossref] [PubMed]
- Engelhardt KE, DeCamp MM, Yang AD, et al. Treatment Approaches and Outcomes for Primary Mediastinal Sarcoma: Analysis of 976 Patients. Ann Thorac Surg 2018;106:333-9. [Crossref] [PubMed]
- Lott-Limbach AA, Wakely PE Jr. Mediastinal sarcomas: experience using fine needle aspiration cytopathology. Mediastinum 2020;4:14. [Crossref] [PubMed]
- Luo DX, Huang MJ, Xiong B, et al. Primary mediastinal sarcoma: surgical outcomes of 21 cases. Interact Cardiovasc Thorac Surg 2013;17:982-6. [Crossref] [PubMed]
- Paquette M, Truong PT, Hart J, et al. Primary sarcoma of the mediastinum: a report of 16 cases referred to the British Columbia Cancer Agency. J Thorac Oncol 2010;5:898-906. [Crossref] [PubMed]
- Fyfe AI, Huckell VF, Burr LH, et al. Leiomyosarcoma of the left atrium: case report and review of the literature. Can J Cardiol 1991;7:193-6. [PubMed]
- Almeida JM. Leiomyosarcoma of the esophagus. Chest 1982;81:761-3. [Crossref] [PubMed]
- Gyhra AS, Santander CK, Alarcón EC, et al. Leiomyosarcoma of the pulmonary veins with extension to the left atrium. Ann Thorac Surg 1996;61:1840-1. [Crossref] [PubMed]
- Eng J, Murday AJ. Leiomyosarcoma of the pulmonary artery. Ann Thorac Surg 1992;53:905-6. [Crossref] [PubMed]
- Chen F, Muranishi Y, Minakata K, et al. Complete resection of a giant mediastinal leiomyosarcoma. Ann Thorac Surg 2015;99:e69-71. [Crossref] [PubMed]
- Moran CA, Suster S, Perino G, et al. Malignant smooth muscle tumors presenting as mediastinal soft tissue masses. A clinicopathologic study of 10 cases. Cancer 1994;74:2251-60. [Crossref] [PubMed]
- Van Schil PE, Colpaert CG, Van Look R, et al. Primary mediastinal leiomyosarcoma. Thorac Cardiovasc Surg 1993;41:377-8. [Crossref] [PubMed]
- Eroğlu A, Kürkçüoğlu C, Karaoğlanoğlu N, et al. Primary leiomyosarcoma of the anterior mediastinum. Eur J Cardiothorac Surg 2002;21:943-5. [Crossref] [PubMed]
Cite this article as: Collaud S, Aigner C. A case report of a giant middle mediastinal leiomyosarcoma. Mediastinum 2022;6:38.