
Thoracoscopic resection of a cavernous haemangioma of anterior mediastinum: case report and literature review
Highlight box
Key findings
• We found that a mediastinal haemangioma can be completely resected under minimally invasive thoracoscopy, which is a safe and reliable procedure relative to traditional open surgery and accelerates patient recovery without postoperative recurrence or metastasis.
What is known and what is new?
• Mediastinal haemangiomas are a rare type of mediastinal tumour, typically benign, are located anterior mediastinum, and lack of specific symptoms and relevant imaging features.
• We herein report a case of thoracoscopic resection of cavernous haemangioma in the anterior mediastinum that was completely resected by thoracoscopy. Although such tumours are mostly benign and the prognosis is good, we recommend aggressive surgical management to avoid missing malignant lesions.
What is the implication, and what should change now?
• We recommend surgical treatment for mediastinal haemangioma to prevent compression symptoms caused by excessive tumour size. Thoracoscopic surgery is minimally invasive, safe and reliable, and should be the first choice of surgical approach.
Introduction
Mediastinal haemangiomas are rare tumours, and some reports indicate that they account for 0.5% or less of all mediastinal tumours (1). Given its nonspecific imaging manifestations, preoperative diagnosis is difficult, and surgery is the main treatment. We herein report a case of cavernous haemangioma in the anterior mediastinum that was successfully treated by video-assisted thoracoscopic surgery (VATS). We present this case in accordance with the CARE reporting checklist (available at https://med.amegroups.com/article/view/10.21037/med-23-1/rc).
Case presentation
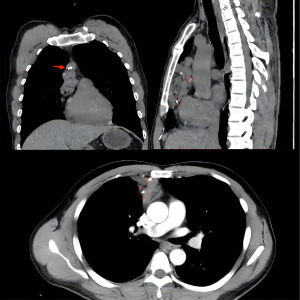
A 40-year-old patient underwent chest computed tomography (CT) during a routine medical examination, and an anterior mediastinal mass was detected. The patient had undergone fracture fixation one year earlier for a right calcaneal fracture, and the internal fixation in the calcaneus was not removed. Otherwise, the patient had no other past medical history, his physical examination and laboratory data were normal, he had no history of chronic or genetic disease, and a chest radiograph showed no abnormalities. A CT scan revealed that a mediastinal mass was located in the anterior mediastinum. The mass range was approximately 9.2 cm × 3.9 cm × 3.6 cm. The CT scan also showed that the mass had a smooth surface and heterogeneous contents. The upper border of the tumour was from the sternal angle and the inferior border of the tumour was at the aortic outflow. The contrast-enhanced CT scan revealed uneven delayed enhancement shadows with multiple punctate calcifications (Figure 1). The patient was unable to undergo magnetic resonance imaging (MRI) due to the internal fixation in the right calcaneus. According to preoperative examinations and imaging reports, we suspected that the mass in the anterior mediastinum was a haemangioma. Mediastinal haemangiomas require differentiation from mediastinal cysts, neurogenic tumours, teratomas, and lymphomas. For diagnosis and treatment, we performed a minimally invasive thoracoscopic mediastinal tumour resection and sent the resected tumour for postoperative pathological examination. After the patient received general anaesthesia and a double lumen endotracheal tube was placed, we introduced a thoracoscope using a trocar in the seventh intercostal space at the posterior axillary line. We placed two other working trocars in the third and sixth intercostal spaces at the anterior axillary line in order to insert the dissecting instruments. The mass was located in the anterior mediastinum encased in a vascular cluster (Figure 2). We opened the mediastinal pleura with an electrocoagulation hook, and the anterior mediastinal haemangioma was resected along the mediastinal adipose tissue. We found that the tumour adhered closely to the superficial pericardium vessels and likely served as a source of vascular supply for the tumour; therefore, these vessels were carefully removed by dissection and the total thoracoscopic resection of the suspected mediastinal haemangioma was complete.
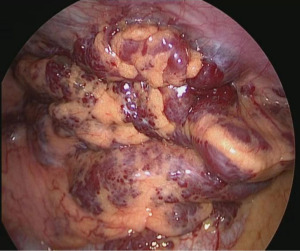
The resected specimen measured 15.0 cm × 6.0 cm × 1.4 cm and was surrounded by pericardial adipose tissue and haemorrhagic and transparent thrombosis (Figure 3). A large number of thick, sponge-like vascular sinuses were found during the mirror-image inspection of the tumour. Based on these findings, the tumours were diagnosed as mediastinal sponge haemangiomas. The patient recovered without postoperative complications and was discharged post-operative day four. The patient was examined one month later, with follow-up visits scheduled every 6 months thereafter. At present, 24 months after surgery, no recurrence has been observed and the individual continues to be carefully monitored as an outpatient. The patient has recovered well and is able to perform heavy physical work without reporting any adverse effects or complications. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.

Discussion
Mediastinal haemangioma is a rare type of mediastinal tumour. The first case was reported by Shennan in 1914 (2), and fewer than 100 cases were reported by the 1980s. The widespread use of CT and MRI technologies has led to an increasing number of cases being identified and reported. However, an up-to-date account of the total number of cases has not been reported in the literature. Instead, several single clinical centre case reports or single centre summaries in different countries and regions have been published. The total number and incidence of mediastinal haemangiomas remain rare compared with other types of mediastinal tumours. Mediastinal haemangiomas are mostly benign and are mainly classified as cavernous or capillary haemangiomas, followed by rarer benign types, including fibroangioma, angiolipoma, fibroangiolipoma, angiolymphangioma, venous haemangioma, arteriovenous fistula and angioleiomyoma (3,4).
Mediastinal haemangiomas are common in the anterior or posterior mediastinum and rarely occur in the middle mediastinum. Approximately 68% of mediastinal haemangiomas are located in the anterior mediastinum, 22% in the posterior mediastinum, and less than 10% are found in the middle mediastinum (5). Patients with mediastinal haemangioma do not present with specific clinical symptoms, and approximately 1/2–1/3 of lesions are discovered incidentally during physical examination by chest X-ray or CT. If symptoms are reported, tumour compression or the invasion of surrounding organs or tissues are often noted, with common symptoms including cough, wheezing, dyspnoea (6), chest pain, hoarseness, superior vena cava obstruction, Horner syndrome or dysphagia caused by the compression of the oesophagus (7), and tumour invasion of the spinal canal (8), which may present with neurological symptoms related to spinal cord compression.
Mediastinal haemangioma is often nonspecific on X-ray and CT imaging. The chest X-ray showed that the haemangioma was a round or lobulated mass. The presence of phleboliths in the lesion was found to be diagnostic, since this feature appears in 10% of patients with mediastinal haemangiomas (3). Moreover, thrombus in the haemangioma, venous inflammation and calcification form phleboliths that appear as rings or spotty calcifications on chest radiography. If the haemangioma is adjacent to the ribs, manifestations of erosion are observed in the ribs. Malignant mediastinal haemangiomas, which show ill-defined and peripheral invasion, can also erode the chest wall. A haemangioma typically appears as a heterogeneous lesion on an unenhanced CT scan, while the degree of internal enhancement of mediastinal haemangioma is heterogeneous on examination with contrast-enhanced chest CT. The degree of central enhancement is significantly higher than that at the edge, which may be a specific manifestation of haemangioma (9). Significant draining veins with local dilatation or venous aneurysm can be found on contrast-enhanced CT. The walls of the draining veins and feeding arteries in the lesion are smooth and regular, which may help to identify other blood-rich malignant tumours that are invading the blurred and irregular vascular wall. Blood supply arteries and draining veins are the main factors that increase the significant risk of bleeding and blood loss (10), and preoperative contrast-enhanced CT reveals draining veins, which are very important for surgical planning. In this case, the feeding artery and drainage vein of the haemangioma were clearly visible by preoperative chest enhanced CT, which allowed thoracoscopic surgery to proceed smoothly.
Chest MRI examination is helpful for imaging-based diagnosis of mediastinal haemangioma, and the findings obtained through magnetic resonance are similar to those of hepatic haemangioma. These lesions have a low to moderate signal intensity on T1-weighted images and high signal intensity on T2-weighted images (11). These characteristics can be attributed to the high vascular space content of haemangiomas. Haemangiomas exhibit three enhancement patterns on postcontrast images: homogeneous enhancement and peripheral nodular enhancement with or without centripetal enhancement. Mediastinal haemangiomas are mostly benign tumours with a low risk of recurrence and metastasis, so positron emission tomography-CT (PET-CT) is not recommended during routine examination unless there is a clear basis for malignancy or the presence of a high-risk factor for malignancy.
Diagnosing mediastinal haemangioma is difficult before surgery because the characteristic features of diagnostic imaging are poor, and these lesions are rarely encountered in clinical practice. Given the lack of specificity, benign haemangiomas are generally caused by congenital dysplasia, mediastinal haemangioma, and haemangioma in other parts of the body and are mainly associated with vascular neoplastic proliferation. Generally, fibrous adipose tissue is also observed to be associated with thymic remnants. Because mediastinal haemangioma is extremely rare in clinical practice and lacks specific clinical manifestations and imaging signs, it is often misdiagnosed as a common mediastinal disease, such as thymoma or neurogenic tumours (12). Imaging findings of significant enhancement and abundance may indicate the possibility of vasogenic tumours, but attention should be given to differentiating these lesions from giant lymphadenopathy, with diagnosis made on the basis of histopathological examination. The most reliable practice is to perform surgical resection and obtain pathological specimens. Because there are many vessels in mediastinal haemangiomas and some tumours are located in the posterior mediastinum or next to the great arteries, preoperative biopsy is not recommended, since this increases the risk of bleeding. For lesions that are difficult to identify, the vascular component should be identified and immunohistochemical assessment should be performed. To exclude lymphangioma and diagnose haemangioma, CD31 and CD34 show positive expression, and D240 shows negative expression (13).
Mediastinal haemangiomas are treated by surgical resection. The traditional surgical approach uses posterolateral, sternotomy or midline incision thoracotomy. In the current case study, preoperative chest CT and MRI examinations were routinely performed to assess the extent of tumour involvement and the course of tumour nutrient vessels in detail, and the appropriate surgical approach and steps were selected to avoid massive haemorrhage caused by blind operation. The development of VATS has led to the use of this technique as a treatment option. At present, there have been many reports on the use of VATS for the complete resection of anterior (posterior) mediastinal haemangiomas (14,15). Compared with the previous approach involving open surgery and resection (16), we achieved complete resection by thoracoscopy. The feeding vessels of the tumour were determined based on preoperative imaging and intraoperative exploration, which was helpful diagnosing and resecting the haemangioma. These observations help ensure proper management and prevent complications, such as bleeding. Thoracoscopic surgery facilitates the satisfactory observation of tumours and blood vessels and can safely remove mediastinal venous haemangiomas. In a retrospective analysis of 18 cases of mediastinal haemangioma (17), all cases were treated with surgical resection, 8 underwent VATS, and 9 underwent traditional posterolateral open surgery, all of which were completely resected without recurrence. This retrospective study confirms that the VATS technique is safe and reliable for performing surgical procedures for mediastinal haemangioma, enabling complete resection and reducing postoperative complications. VATS resulted in the complete resection of the anterior mediastinal haemangioma in this patient without bleeding or other complications. We suggest that, with a thorough preoperative examination and skilled operation, thoracoscopic complete resection is safe and feasible with less trauma to patients, rapid postoperative recovery and can reduce the occurrence of complications, such as bleeding. Several retrospective analyses (4,17) have reported that a very small number of patients with mediastinal haemangiomas experience recurrence after surgery due to incomplete resection or a higher degree of malignancy with an overall better prognosis. Although mediastinal haemangiomas are mostly benign and have a very low probability of recurrence, relevant research or guidelines are not available to indicate whether mediastinal haemangiomas require monitoring. We recommend that patients with mediastinal haemangioma undergo CT after surgery to prevent tumour recurrence, but further studies are required.
Conclusions
In summary, mediastinal haemangioma is a rare mediastinal tumour, most of which is benign, in the anterior mediastinum, and lacks specific symptoms and relevant imaging features. VATS is safe and reliable compared with the traditional thoracotomy approach. Although such diseases are mostly benign and the prognosis is good, we still recommend aggressive surgical management to avoid missing malignant lesions.
Acknowledgments
We thank the 2022 Chinese Congress on Oncology for its support and encouragement and for providing the authors with the opportunity to share this case. We thank the Mediastinal Committee of China Anti-Cancer Association for their guidance on this paper. Some content in this article has been presented in speech form by the authors at the 2022 Chinese Congress on Oncology Mediastinal Tumor Conference. This article was submitted to Mediastinum as a conference submission.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://med.amegroups.com/article/view/10.21037/med-23-1/rc
Peer Review File: Available at https://med.amegroups.com/article/view/10.21037/med-23-1/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-23-1/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work and will ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wada H, Teramatsu T. Mediastinal tumors--a statistical nationwide report of 1,546 cases between July, 1975 and May, 1979 in Japan (author's transl). Nihon Kyobu Geka Gakkai Zasshi 1982;30:374-8. [PubMed]
- Shennan T. Histologically non-malignant angioma with numerousmetastases. J Pathol Bacteriol 1914;19:139-54. [Crossref]
- Davis JM, Mark GJ, Greene R. Benign blood vascular tumors of the mediastinum. Report of four cases and review of the literature. Radiology 1978;126:581-7. [Crossref] [PubMed]
- Yasuda A, Mizuno A, Mishima A, et al. Posterior mediastinal angioleiomyoma: report of a case. J Thorac Imaging 2007;22:363-5. [Crossref] [PubMed]
- Yoshino N, Okada D, Ujiie H, et al. Venous hemangioma of the posterior mediastinum. Ann Thorac Cardiovasc Surg 2012;18:247-50. [Crossref] [PubMed]
- Deepak J, Babu MN, Gowrishankar BC, et al. Mediastinal hemangioma: Masquerading as pleural effusion. J Indian Assoc Pediatr Surg 2013;18:162-4. [Crossref] [PubMed]
- Odaka M, Nakada T, Asano H, et al. Thoracoscopic resection of a mediastinal venous hemangioma: Report of a case. Surg Today 2011;41:1455-7. [Crossref] [PubMed]
- Callahan WJ, Simon AL. Posterior mediastinal hemangioma associated with vertebral body hemangioma. J Thorac Cardiovasc Surg 1966;51:283-5. [Crossref] [PubMed]
- McAdams HP, Rosado-de-Christenson ML, Moran CA. Mediastinal hemangioma: radiographic and CT features in 14 patients. Radiology 1994;193:399-402. [Crossref] [PubMed]
- Li JL, Liu HJ, Cui YH, et al. Mediastinal hemangiomas: Spectrum of CT and MRI findings - retrospective case series study and systematic review of the literature. Eur J Radiol 2020;126:108905. [Crossref] [PubMed]
- Park JW, Jeong WG, Lee JE, et al. Pictorial Review of Mediastinal Masses with an Emphasis on Magnetic Resonance Imaging. Korean J Radiol 2021;22:139-54. [Crossref] [PubMed]
- Zeyaian B, Soleimani N, Geramizadeh B. Posterior mediastinal capillary hemangioma misdiagnosed as neurofibromas: a rare case report and review of the literature. Rare Tumors 2015;7:5639. [Crossref] [PubMed]
- Kahn HJ, Bailey D, Marks A. Monoclonal antibody D2-40, a new marker of lymphatic endothelium, reacts with Kaposi's sarcoma and a subset of angiosarcomas. Mod Pathol 2002;15:434-40. [Crossref] [PubMed]
- Maeda S, Takahashi S, Koike K, et al. Preferred surgical approach for dumbbell-shaped tumors in the posterior mediastinum. Ann Thorac Cardiovasc Surg 2011;17:394-6. [Crossref] [PubMed]
- Chan AP, Wong RH, Wan IY, et al. Video-assisted thoracic surgery excision of mediastinal hemangioma. Asian Cardiovasc Thorac Ann 2009;17:522-4. [Crossref] [PubMed]
- Cohen AJ, Sbaschnig RJ, Hochholzer L, et al. Mediastinal hemangiomas. Ann Thorac Surg 1987;43:656-9. [Crossref] [PubMed]
- Xu X, Qin X, Yang B, et al. Surgical management of mediastinal hemangioma: a report of 18 cases. Chinese Journal of Thoracic and Cardiovascular Surgery 2018;34:818-21.
Cite this article as: Xu J, Xu Y, Zhang R. Thoracoscopic resection of a cavernous haemangioma of anterior mediastinum: case report and literature review. Mediastinum 2023;7:30.


