
Resection of a giant mediastinal liposarcoma by median sternotomy with vascular reconstruction—a case report
Highlight box
Key findings
• Extended resection and vascular reconstruction for the surgical treatment of primary mediastinal liposarcoma is often necessary to ensure adequate radicality and to reduce the risk of local recurrence.
What is known and what is new?
• Primary mediastinal liposarcomas are rare but associated with local aggressive biological behavior. Despite, they are often diagnosed as an incidental finding without any symptoms.
• Here we describe the case of a 69-year-old female patient with a large mass in the anterior mediastinum suggestive for mediastinal liposarcoma. Primary tumor resection with “en bloc” resection of the innominate vein with vascular graft reconstruction was performed. The postoperative course was uneventful. Six months follow-up after surgery showed no signs of local recurrence or dissemination.
What is the implication, and what should change now?
• Patients with mediastinal liposarcomas should be investigated and treated by an interdisciplinary team in high-volume centers with sufficient experience. Extensive resections and broncho-vascular reconstructions can become the standard in the treatment of locally advanced primary mediastinal liposarcoma in high-volume centers with the aim of improving the control of local recurrence and overall survival.
Introduction
Thoracic location of well-differentiated liposarcoma is extremely rare (1-4). These tumours are locally aggressive with risk of recurrence but good prognosis as metastases is rare (5). Due to its anatomical location the tumor is commonly associated with infiltration of surrounding structures (6). These tumors are often diagnosed as incidental findings without any symptoms. Here we would like to present a case of the huge mediastinal liposarcoma with typical diagnostic pitfalls treated with extended resection of the pericardium and left innominate vein followed by vascular reconstruction to achieve adequate resection margins and restoration of the original anatomical arrangement with reconstruction of the venous return. We present this case in accordance with the CARE reporting checklist (available at https://med.amegroups.com/article/view/10.21037/med-23-20/rc) (7).
Case presentation
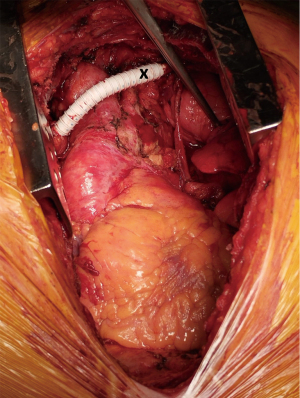
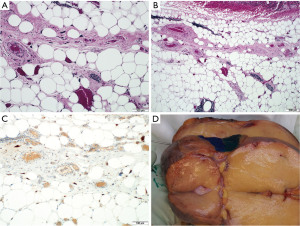
A 69-year-old female patient was examined for an unclear upper respiratory tract infection associated with a prolonged dry cough. Chest X-ray revealed a huge mass in the anterior mediastinum and the patient was referred to our department for further treatment. Analysis of past medical history showed previous thyroidectomy with subsequent hypocalcaemic crises due to secondary hypoparathyroidism with calcium replacement therapy, large bowel diverticulosis, mild aortic stenosis and microangiopathic leukoencephalopathy. The family medical history was unremarkable. The physical examination showed no further abnormality. The patient had no history of fever, hemoptysis, excessive night sweating or significant weight loss. Standard laboratory testing of blood and tumor markers found no deviation from [alpha-fetoprotein 1.9 µg/L, beta-human chorionic gonadotropin (beta-HCG) 2.7 U/L] the norm except for a slight increase of beta-2-microglobulin (2.52 mg/L). Subsequent contrast enhanced computed tomography (CT) scan confirmed a huge tumor of the anterior mediastinum measuring 28 cm × 22 cm with extension into both pleural cavities with fat density [−112 to −14 Hounsfield units (HU)] and infiltration of the pericardium and the left brachiocephalic vein (Figure 1). Ultrasound-guided biopsy confirmed the presence of fat cells in the tumor mass, but without clear signs of malignant transformation. Based on the imaging results suggesting liposarcomatous radiomorphology, the patient was presented in a multidisciplinary tumor board, where surgical resection was indicated. The median sternotomy was considered as an appropriate approach given the size and location of the tumor. Intraoperatively, in correlation with CT, a sharply defined mass of lipomatous consistency was found substernally with extension to the left pleural cavity, but without intrapleural infiltration. During the operation, it was necessary to remove the entire anterior wall of the pericardium with subsequent replacement using polyglactin mesh 25 cm × 15 cm (to prevent cardiac herniation) and “en bloc” resection of the innominate vein with vascular reconstruction using 8 mm polytetrafluoroethylene (PTFE) graft. Prior to vascular resection 5,000 international units (IU) heparin was administered (Figure 2). Vascular anastomoses of the artificial prosthesis between the subclavian vein and the superior vena cava were performed using a running 5/0 polypropylene suture. Operative time was 195 min and intraoperative blood loss was 750 mL. No blood transfusion was required intra- or postoperatively. The patient was postoperatively successfully extubated, and the further course was uneventful. Chest drainages were removed on the fifth postoperative day (POD 5) and the patient was discharged on POD 9. Histopathologic examination showed the tumor composed of mature adipose tissue with marked variability of cell size and scattered atypical spindle cells with bizarre hyperchromatic nuclei and rarely present of fine fibrous septa in intercellular space. Immunohistochemical testing showed mouse double minute-2 homolog (MDM2) and CDK4 positivity, confirming the presumptive diagnosis of primary mediastinal well-differentiated liposarcoma (Figure 3). Considering the tumor diameter without nodal involvement and good differentiation, the tumor was classified as T4N0M0 in the stage IB according to latest tumor, node, metastasis (TNM) classification (2). No adjuvant therapy was indicated. Six months follow-up after surgery with CT scan showed no signs of local recurrence or dissemination (Figure 4). Anticoagulant therapy after vascular reconstruction was discontinued after three months. All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.


Discussion
Liposarcoma is a very rare malignancy of mesenchymal origin, firstly reported by Virchow in 1857 (8). To the best of our knowledge, less than 200 cases of intrathoracic liposarcoma have been so far published in the literature (6). The symptomatology of the disease is nonspecific and conditioned by compression or invasion of adjacent structures, such as cough, dyspnea, dysphagia, superior vena cava syndrome or progressive heart failure. In contrary, an asymptomatic course with incidental finding is not uncommon (9,10). These tumors occur mainly in the posterior mediastinum, followed by the anterior, and most rarely in the middle part of the mediastinum (11). Intrapulmonary growth has also been reported in rare cases (12). CT scan is the gold standard in non-invasive mediastinal diagnostics. Liposarcoma is characterized by negative HU values in CT imaging (ranging from approximately −80 to +40) and negative the HU values correlate with a higher the degree of differentiation (11,13). In our case of a well-differentiated liposarcoma HU values ranged from −112 to −14. Magnetic resonance (MR) imaging is not routinely performed, however is probably the best modality to distinguish between cystic and solid mediastinal masses and to evaluate soft tissue involvement (14). The use of 2-Deoxy-2-[18F] fluoro-D-glucose positron emission tomography (PET)/CT (18FDG PET/CT) in the diagnosis of primary mediastinal lesions is considered as an additional examination. Highly PET-avid tumors are generally considered to be tumors with a lower degree of differentiation (15). The World Health Organization (WHO) classification divides liposarcoma into 4 subtypes: well-differentiated, dedifferentiated, myxoid/round cell and pleomorphic (16). Dedifferentiated and pleomorphic subtype have a poor prognosis (6). Like well-differentiated liposarcoma dedifferentiated Liposarcoma show amplification of CDK4 and MDM2. MDM2 and CDK4 represent tumor suppressor genes localized on the twelfth chromosome. Deregulation and overexpression of MDM2, CDK4 promoting tumorigenesis by dysregulation of apoptotic p53 pathway (1). The amplification of these two genes is accepted as a diagnostic criterion for distinguishing well-differentiated liposarcoma from lipoma which can be a diagnostic pitfall, as our presented case has shown (1,6,16). Chemoresistance and low radiosensitivity of tumors arising from mesenchymal origin favor surgical approach as the only option for radical treatment (17). Surgical resection is therefore the most common treatment strategy for mediastinal liposarcoma. Small lesions without prior histological verification may be resected by a minimally invasive approach, but large tumors usually require open access. As in our case of large mediastinal tumor, fine needle biopsy is usually recommended for histological verification prior to surgery. According to the available literature, the risk of needle tract seeding is very low and negligible. Although en bloc excision of the needle tract with the primary tumor can be performed, the evidence for improved oncologic outcomes is lacking (18). Previous case presentations have reported a variety of surgical approaches; however incision should be adopted to the location of the lesion (13,17,19). Median sternotomy represents a standard approach to anterior mediastinal tumors and can be extended to both sides in terms of hemiclamshell or clamshell incision and can be used for initiation of extracorporeal circulation if necessary (20). Extensive vascular and bronchoplastic resections and reconstructions of adjacent mediastinal organs such as the heart or esophagus are described very rarely in the literature (17,19). Surgical radicality is a crucial prerequisite for successful therapeutic outcome. Adjuvant therapy is generally considered in patients at an increased risk of local recurrence so that improved local control may be achieved (21,22). In mediastinal liposarcoma, there is no consensus on the use of radiotherapy postoperatively, however in a small number of patients, the benefit of postoperative radiation therapy in retroperitoneal liposarcoma has been demonstrated (23). On the other hand, the potentially negative consequences of radiation therapy of the mediastinum on lung and heart tissues have to be considered as well (24). Chemotherapy is generally ineffective for liposarcoma, but molecular analysis showed that part of the well-differentiated and dedifferentiated liposarcomas expressed programmed death ligand-1 (PD-L1) and theoretically could benefit from the use of immune-checkpoint inhibitors. The potential clinical efficacy still needs to be assessed in clinical trials in the future (11,25). Angiogenesis inhibitors showed promising results in a phase 3 study (26).
Conclusions
Primary mediastinal liposarcoma is a rare tumor and radical surgery represents the treatment of choice. Due to its location, and infiltrative growth, extended resection and vascular reconstruction is often necessary to ensure radical resection and to reduce the probability of local recurrence. Therefore, these patients should be treated in high-volume centers with sufficient experience.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://med.amegroups.com/article/view/10.21037/med-23-20/rc
Peer Review File: Available at https://med.amegroups.com/article/view/10.21037/med-23-20/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-23-20/coif). M.H. receives payments or Honoraria for lectures or presentations from AstraZeneca, Boehringer Ingelheim, MSD, Roche, and Lilly. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Suster DI. The role of molecular pathology in mediastinal sarcomas. Mediastinum 2020;4:33. [Crossref] [PubMed]
- Cates JMM. The AJCC 8th Edition Staging System for Soft Tissue Sarcoma of the Extremities or Trunk: A Cohort Study of the SEER Database. J Natl Compr Canc Netw 2018;16:144-52.
- Paquette M, Truong PT, Hart J, et al. Primary sarcoma of the mediastinum: a report of 16 cases referred to the British Columbia Cancer Agency. J Thorac Oncol 2010;5:898-906. [Crossref] [PubMed]
- Hahn HP, Fletcher CD. Primary mediastinal liposarcoma: clinicopathologic analysis of 24 cases. Am J Surg Pathol 2007;31:1868-74. [Crossref] [PubMed]
- Tsao MS, Nicholson AG, Maleszewski JJ, et al. Introduction to 2021 WHO Classification of Thoracic Tumors. J Thorac Oncol 2022;17:e1-4. [Crossref] [PubMed]
- Kiełbowski K, Ruszel N, Skrzyniarz SA, et al. Clinicopathological Features of Intrathoracic Liposarcoma-A Systematic Review with an Illustrative Case. J Clin Med 2022;11:7353. [Crossref] [PubMed]
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Kim YB, Leem DH, Baek JA, et al. Atypical lipomatous tumor/well-differentiated liposarcoma of the gingiva: a case report and review of literature. J Oral Maxillofac Surg 2014;72:431-9. [Crossref] [PubMed]
- Nguyen DC, Olatubosun O, Yu W, et al. Giant Mediastinal Liposarcoma: A Rare Yet Distinct Clinical Entity. Ann Thorac Surg 2018;106:e117-9. [Crossref] [PubMed]
- Miura K, Hamanaka K, Matsuoka S, et al. Primary mediastinal dedifferentiated liposarcoma: Five case reports and a review. Thorac Cancer 2018;9:1733-40. [Crossref] [PubMed]
- Wong GS, Bass D, Chen IY, et al. Imaging and Clinical Findings in a Series of Six Cases of Rare Primary Mediastinal Liposarcoma. Radiol Cardiothorac Imaging 2022;4:e210259. [Crossref] [PubMed]
- Collaud S, Stork T, Schildhaus HU, et al. Multimodality treatment including surgery for primary pulmonary sarcoma: Size does matter. J Surg Oncol 2020;122:506-14. [Crossref] [PubMed]
- Zhang H, Yimin N, He Z, et al. Giant mediastinal liposarcoma resected by median sternotomy: a case report. Transl Cancer Res 2020;9:6522-7. [Crossref] [PubMed]
- Carter BW, Benveniste MF, Marom EM. Diagnostic approach to the anterior/prevascular mediastinum for radiologists. Mediastinum 2019;3:18. [Crossref] [PubMed]
- Tatci E, Ozmen O, Dadali Y, et al. The role of FDG PET/CT in evaluation of mediastinal masses and neurogenic tumors of chest wall. Int J Clin Exp Med 2015;8:11146-52. [PubMed]
- Sbaraglia M, Bellan E, Dei Tos AP. The 2020 WHO Classification of Soft Tissue Tumours: news and perspectives. Pathologica 2021;113:70-84. [Crossref] [PubMed]
- Zhang M, Zhang S, Shi H, et al. Resection of a huge mediastinal well-differentiated liposarcoma involving left thoracic cavity. J Cardiothorac Surg 2019;14:148. [Crossref] [PubMed]
- Van Houdt WJ, Schrijver AM, Cohen-Hallaleh RB, et al. Needle tract seeding following core biopsies in retroperitoneal sarcoma. Eur J Surg Oncol 2017;43:1740-5. [Crossref] [PubMed]
- Billè A, Garofalo G, Leo F, et al. Giant liposarcoma elongating mediastinal vessels with intrathoracic inferior vena cava replacement. Eur J Cardiothorac Surg 2013;44:570-2. [Crossref] [PubMed]
- Toda M, Izumi N, Tsukioka T, et al. Huge mediastinal liposarcoma resected by clamshell thoracotomy: a case report. Surg Case Rep 2017;3:16. [Crossref] [PubMed]
- Marjiyeh-Awwad R, Mansour S, Khuri S. Giant Retroperitoneal Liposarcoma: Correlation Between Size and Risk for Recurrence. World J Oncol 2022;13:244-8. [Crossref] [PubMed]
- Salerno KE. Radiation Therapy for Soft Tissue Sarcoma: Indications, Timing, Benefits, and Consequences. Surg Clin North Am 2022;102:567-82. [Crossref] [PubMed]
- Lee HS, Yu JI, Lim DH, et al. Retroperitoneal liposarcoma: the role of adjuvant radiation therapy and the prognostic factors. Radiat Oncol J 2016;34:216-22. [Crossref] [PubMed]
- Benveniste MF, Gomez D, Carter BW, et al. Recognizing Radiation Therapy-related Complications in the Chest. Radiographics 2019;39:344-66. [Crossref] [PubMed]
- Chae H, Kim JE, Kim W, et al. Clinicopathologic Characteristics and Clinical Outcome of Localized Liposarcoma: A Single-Center Experience over 25 Years and Evaluation of PD-L1 Expression. Cancer Res Treat 2022;54:579-89. [Crossref] [PubMed]
- Schöffski P, Chawla S, Maki RG, et al. Eribulin versus dacarbazine in previously treated patients with advanced liposarcoma or leiomyosarcoma: a randomised, open-label, multicentre, phase 3 trial. Lancet 2016;387:1629-37. [Crossref] [PubMed]
Cite this article as: Benej M, Klikovits T, Krajc T, Watzka S, Hochmair M, Krenbek D, Aigner C. Resection of a giant mediastinal liposarcoma by median sternotomy with vascular reconstruction—a case report. Mediastinum 2023;7:39.


