
Modified subxiphoid thoracoscopic thymectomy for early-stage thymic tumor: case report
Introduction
Minimally invasive thymectomy via subxiphoid approach has some obvious advantages over the traditional lateral thoracic approach: it is easier to reveal the phrenic nerve on both sides and to obtain better surgical field (1,2). However, due to the narrow operating space behind the sternum, the application of the subxiphoid thoracoscopic thymectomy can be subject to some limitations, such as the tendency to hemorrhage and the difficulty in achieving total thymectomy. In order to solve this problem, Zieliński et al. (1) reported an operative technique of a transcervical subxiphoid thoracoscopic thymectomy to increase the space behind the sternum, but the surgical invasiveness of this method has limited its widespread use. Here we add a sternal retractor to elevate the sternum above the traditional subxiphoid approach to obtain a larger surgical operating space, which makes the subxiphoid thoracoscopic thymectomy easier to perform and thus improves the safety of the procedure (3).
The technique of modified subxiphoid thoracoscopic thymectomy described here is that which is now routinely employed in the Department of Thoracic Surgery at the Zhongshan Hospital of Fudan University (Video 1). We present this article in accordance with the CARE reporting checklist (available at https://med.amegroups.com/article/view/10.21037/med-21-23/rc).
Case presentation
Clinical summary
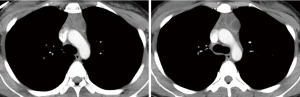
A 27-year-old female patient presented with an incidental finding of a thymic mass on plain chest computed tomography (CT). Further chest contrast CT revealed a 35 mm × 25 mm lesion in the anterior mediastinum which might be adherent to the left innominate vein (Figure 1). The CT diagnosis was teratoma. The serum alpha fetoprotein (AFP) level was 3.4 ng/mL, and serum beta human chorionic gonadotropin (β-HCG) level was <0.1 mIU/mL. No puncture biopsy was performed in this patient. There was no relative past medical history with the thymic mass.
Pre-operative assessment
The patient was in good general health, except for this thymic mass. Her menstruation was regular and she was not in her menstrual period at that time. Her heart and lung function were in good condition, and no contraindications to surgery were found. The neurologist evaluated this patient for the absence of myasthenia gravis.
Anaesthesia and positioning
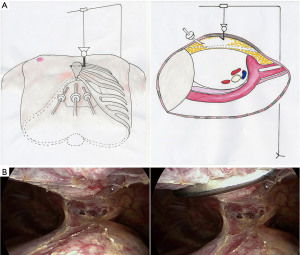
The patient was placed in the supine position with the legs spread apart in a scissors position to allow the surgeon to stand for the procedure. After general anesthesia induction, single-lumen endotracheal tube was inserted to conduct lung ventilation in the procedure. A sternal retractor device was installed on the operating table in preparation for the installation of a sternal retractor to elevate the sternum (Figure 2A).
Technique
The procedure was the same as for modified subxiphoid thoracoscopic thymectomy as described by our previous study (3), with the key points detailed here. First of all, a 2.0–2.5 cm transverse skin incision was made in the subxiphoid position to place the high-definition thoracoscope. The surgeon used the fingers to fully free the posterior sternal space and the bilateral costal arch space. Two 1.0 cm incisions were made at the bilateral costal arch 5.0–10.0 cm away from the subxiphoid incision to insert the surgical instruments. The pleura on both sides of the anterior mediastinum was incised with an ultrasonic scalpel. The posterior sternal space was mobilized with ultrasonic scalpel up to the level of the second intercostal space. A 1.0 cm transverse skin incision was made at the third intercostal parasternal position to insert a sternal retractor fixed to the sternal retractor device to elevate the sternum. Carbon dioxide was charged into the chest cavity via the thoracoscopic trocar to lower the lungs.
By following above steps, a better surgical view was obtained (Figure 2B). Ultrasonic scalpel was used to mobilize the lower pole of the thymus. Using the phrenic nerves on both sides as the boundary, all thymic tissue between the phrenic nerves was removed, and care was always taken to protect the phrenic nerves on both sides from accidental injury. If the thymic tumor was close to the phrenic nerve, electrocoagulation hook separation was a better option than ultrasonic scalpel. The thymic tissue was further mobilized up to the left innominate vein and then carefully mobilized from the left innominate vein. Ultrasonic scalpel was used to mobilize the upper pole of the thymus and the thymic vein was cut off after clamping with a hem-o-lok vascular clip. After all thymic tissue had been removed, the resected specimen was removed from the subxiphoid incision, the length of which was extended according to the size of the specimen.
Post-operative management
The patient was safely returned to the ward after awakening from anesthesia. She ate and got out of bed on the first day after the surgery and was discharged after the chest tube was removed on the second day after the surgery. The patient felt a little pain and was satisfied with the outcome of the treatment. The pathological diagnosis was mature teratoma.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Thanks to the use of the sternal retractor, modified subxiphoid thoracoscopic thymectomy can obtain a larger posterior sternal space and a better surgical view, thus making the procedure easier and safer. This surgical approach is not only applicable to early-stage thymic tumors, but also to some locally advanced thymic tumors as well (3). Compared with lateral intercostal thoracoscopic thymectomy, the subxiphoid approach provides a better view of the phrenic nerves on both sides to avoid accidental intraoperative injure to the phrenic nerves (4). In addition, this technique permits superior views of the anterosuperior mediastinal space, which is crucial during mobilizing the left innominate vein, thus reducing the probability of accidental bleeding from the left innominate vein (5).
Conclusions
In conclusion, modified subxiphoid thoracoscopic thymectomy using an auxiliary sternal retractor makes minimally invasive thymectomy safer and simpler and is an alternative option for patients with early-stage thymic tumors.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://med.amegroups.com/article/view/10.21037/med-21-23/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-21-23/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zieliński M, Kuzdzał J, Szlubowski A, et al. Transcervical-subxiphoid-videothoracoscopic "maximal" thymectomy--operative technique and early results. Ann Thorac Surg 2004;78:404-9; discussion 409-10. [Crossref] [PubMed]
- Kido T, Hazama K, Inoue Y, et al. Resection of anterior mediastinal masses through an infrasternal approach. Ann Thorac Surg 1999;67:263-5. [Crossref] [PubMed]
- Jiang JH, Gao J, Zhang Y, et al. Modified subxiphoid thoracoscopic thymectomy for locally invasive thymoma. Ann Thorac Surg 2021;112:1095-100. [Crossref] [PubMed]
- Li J, Qi G, Liu Y, et al. Meta-analysis of subxiphoid approach versus lateral approach for thoracoscopic Thymectomy. J Cardiothorac Surg 2020;15:89. [Crossref] [PubMed]
- Numanami H, Yano M, Yamaji M, et al. Nakanishi R, Haniuda M. Thoracoscopic Thymectomy Using a Subxiphoid Approach for Anterior Mediastinal Tumors. Ann Thorac Cardiovasc Surg 2018;24:65-72. [Crossref] [PubMed]
Cite this article as: Jiang JH, Zhang Y, Ding JY. Modified subxiphoid thoracoscopic thymectomy for early-stage thymic tumor: case report. Mediastinum 2023;7:38.


