
Evolution of radiotherapy techniques for mediastinal Hodgkin lymphoma: a single-center experience
Hodgkin lymphoma (HL) is a rare hematological malignancy associated with a high curability rate, ranging between 80% and 90% (1). Limitation of treatment-related toxicities is consequently of prime importance. Consolidation radiation therapy following first-line chemotherapy improves progression-free survival (PFS) for favorable and unfavorable early-stage HL (2); however, first-generation bidimensional (2D) techniques, which used extended fields, largely exposed thoracic organs-at-risk (OAR), leading to an increased risk of late radiation-induced adverse events, such as cardiac failure, pulmonary toxicity and second cancers (3). More recently, target volumes were limited to the initially involved sites and technical progresses were made in order to spare OAR, substantially reducing the delivered integral dose. Such technical developments included intensity-modulated radiation therapy (IMRT) and intensity-modulated proton therapy (IMPT) (4). The aim of this study was to analyze the evolution of the RT techniques for mediastinal HL irradiation in our Department of Radiation Oncology on a period of 17 years between January 2005 and January 2022. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Institut Curie (date: 2112021) and individual consent for this retrospective analysis was waived.
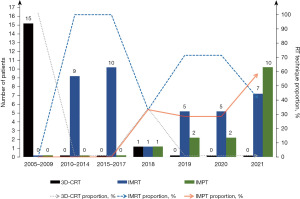
Since 2005, an institutional database records all lymphoma patients referred to the radiation oncologists of our department for radiotherapy planning; the aim of this retrospective study was to describe the technical evolution of consolidative radiotherapy for mediastinal HL irradiation from 2005 to 2022. During this period, 68 new mediastinal HL patients were addressed to our department: of them, 16 were treated with tridimensional conformal radiotherapy (3D-CRT) on a period between 2005 and 2018, 37 were treated with IMRT (either with volumetric modulated arc therapy or helical tomotherapy) which was introduced in this indication in 2010, and 15 were treated with IMPT, which was introduced in this indication in 2018. IMPT was systematically delivered on a gantry with spirometer-controlled deep-inspiration breath hold, based on the involved-site radiation therapy standard, and normofractionated. The proportion of IMPT treatments was 0% before 2018, 33.3% in 2018 (1 patient/3), 28.6% in 2019 (2 patients/7), 28.6% in 2020 (2 patients/7), and 58.8% in 2021 (10 patients/17). The evolution of 3D-CRT, IMRT and IMPT distribution for mediastinal HL irradiation is shown in Table 1 and Figure 1.
Table 1
| Radiotherapy techniques | 2005–2009 | 2010–2014 | 2015–2018 | 2019–2022 |
|---|---|---|---|---|
| All HL patients treated with RT | 15 | 9 | 13 | 31 |
| Patients treated with 3D-CRT | 15 [100] | – | 1 [8] | – |
| Patients treated with IMRT | – | 9 [100] | 11 [85] | 17 [55] |
| Patients treated with IMPT | – | – | 1 [8] | 14 [45] |
Data are presented as n or n [%]. IMRT, intensity-modulated radiation therapy; IMPT, intensity-modulated proton therapy; HL, Hodgkin lymphoma; RT, radiation therapy; 3D-CRT, tridimensional conformal radiotherapy.
The main indications for mediastinal HL proton therapy were young patients (less than 30 years old), considering that the cumulative incidence of secondary cancer increased when the age at first treatment decreased with a long-lasting risk (5), or patients with a significant cardiovascular risk either due to baseline cardiovascular risk factors or to the localization of the initially involved sites in the vicinity of critical cardiac substructures. Among the 15 institutional patients treated with IMPT, 13 were women and the median age was 26 years (range, 18–37 years); there were 12 stage II unfavorable HL, 2 stage II favorable HL, and 1 “grey zone” lymphoma. Median prescription dose was 30 Gy (range, 30–36 Gy). IMPT is expected to significantly reduce radiation exposure to OAR and to improve target coverage compared with IMRT. Based on a dosimetric comparison between IMRT and IMPT, we found that IMPT significantly reduced mean doses to the heart (2.36 vs. 0.99 Gy, P<0.01), to the left ventricle (0.67 vs. 0.03 Gy, P<0.01) and to the valves (1.29 vs. 0.06 Gy, P<0.01) (6). While IMPT treatments are still minoritary in our department and are systematically subject to a dosimetric selection process based on a comparison between optimal IMRT and IMPT plans (7,8), proton therapy has become the main technique for mediastinal HL lymphoma. IMPT is currently facing multiple challenges, such as limited access to proton therapy facilities, reimbursement issues, development of new effective regimens for HL management (such as targeted therapies or immunotherapies) and optimal selection process which is still subject to debate (7). In any case, the National Comprehensive Cancer Network (NCCN) guidelines still consider IMRT/volumetric-modulated arc therapy (VMAT) as a standard technique (9) and the ILROG guidelines on the utilization of IMPT suggest a careful adoption of this latter, taking into account all the physical limitations of IMPT in a delicate and anatomically complex district, as it is the thorax (10).
While a longer follow-up for IMPT is needed to evaluate its efficacy and late toxicity profile, this single-center experience evidences how proton therapy, once only used for highly selected patients, could become a reference technique in the treatment of mediastinal HL patients, despite multiple challenges including limited availability and financial cost.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Mediastinum. The article has undergone external peer review.
Peer Review File: Available at https://med.amegroups.com/article/view/10.21037/med-23-13/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-23-13/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the Institutional Review Board of the Institut Curie (date: 2112021). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cuccaro A, Bartolomei F, Cupelli E, et al. Prognostic factors in hodgkin lymphoma. Mediterr J Hematol Infect Dis 2014;6:e2014053. [Crossref] [PubMed]
- André MPE, Girinsky T, Federico M, et al. Early Positron Emission Tomography Response-Adapted Treatment in Stage I and II Hodgkin Lymphoma: Final Results of the Randomized EORTC/LYSA/FIL H10 Trial. J Clin Oncol 2017;35:1786-94. [Crossref] [PubMed]
- Holtzman AL, Stahl JM, Zhu S, et al. Does the Incidence of Treatment-Related Toxicity Plateau After Radiation Therapy: The Long-Term Impact of Integral Dose in Hodgkin's Lymphoma Survivors. Adv Radiat Oncol 2019;4:699-705. [Crossref] [PubMed]
- Hoppe BS, Hill-Kayser CE, Tseng YD, et al. Consolidative proton therapy after chemotherapy for patients with Hodgkin lymphoma. Ann Oncol 2017;28:2179-84. [Crossref] [PubMed]
- van Leeuwen FE, Ng AK. Long-term risk of second malignancy and cardiovascular disease after Hodgkin lymphoma treatment. Hematology Am Soc Hematol Educ Program 2016;2016:323-30. [Crossref] [PubMed]
- Loap P, Orlandi E, De Marzi L, et al. Cardiotoxicity model-based patient selection for Hodgkin lymphoma proton therapy. Acta Oncol 2022;61:979-86. [Crossref] [PubMed]
- Loap P, De Marzi L, Mirandola A, et al. Development and Implementation of Proton Therapy for Hodgkin Lymphoma: Challenges and Perspectives. Cancers (Basel) 2021;13:3744. [Crossref] [PubMed]
- Loap P, Goudjil F, Dendale R, et al. Clinical and technical considerations for mediastinal Hodgkin lymphoma protontherapy based on a single-center early experience. Cancer Radiother 2021;25:779-85. [Crossref] [PubMed]
- Hoppe RT, Advani RH, Ai WZ, et al. NCCN Guidelines® Insights: Hodgkin Lymphoma, Version 2.2022. J Natl Compr Canc Netw 2022;20:322-34. [Crossref] [PubMed]
- Dabaja BS, Hoppe BS, Plastaras JP, et al. Proton therapy for adults with mediastinal lymphomas: the International Lymphoma Radiation Oncology Group guidelines. Blood 2018;132:1635-46. Erratum in: Blood 2019;133:1384-5. [Crossref] [PubMed]
Cite this article as: Loap P, El Ayachy R, Beddok A, Abbassi L, Boilève A, Deau Fischer B, Willems L, Franchi P, Bouscary D, Kirova Y. Evolution of radiotherapy techniques for mediastinal Hodgkin lymphoma: a single-center experience. Mediastinum 2024;8:10.


