Descending necrotizing mediastinitis: key points to reduce the high associated mortality in a consecutive case series
Highlight box
Key findings
• Descending necrotizing mediastinitis (DNM) is an uncommon but life-threatening infection.
What is known and what is new?
• Rapid diagnosis and aggressive combined medical and surgical treatment could be crucial to reduce the mortality of patients with DNM.
• In addition to the transcervical approach, videothoracoscopic mediastinal drainage is an effective and minimally invasive treatment for DNM with tracheal carinal spread that avoids the morbidity of open drainage.
What is the implication, and what should change now?
• Broad-spectrum antibiotics and timely approach combining cervicotomy and a minimally invasive thoracic approaches may be key to reducing mortality.
Introduction
Descending necrotizing mediastinitis (DNM) is a rare and severe acute infection involving the neck and chest, secondary to odontogenic, pharyngeal, peritonsillar, or other cervical infections that rapidly spread into the mediastinum and thoracic cavities (1). Despite an accurate and timely diagnosis, antibiotic administration, and aggressive surgical treatment, the mortality rate of patients suffering DNM range between 20–40%, mainly due to sepsis and multiple organ dysfunction syndrome (2,3).
The term DNM was first used in 1938 by Pearse (4) when he described how this infection spreads to the mediastinum via the cervical fascial plane, favored by the negative intrathoracic pressure and gravity. Diagnosis is based on the criteria defined by Estrera et al. in 1983 (2): (I) clinical manifestation of severe infection; (II) radiological abnormalities characteristic of the disease; (III) surgical or post-mortem evidence of DNM; and (IV) correlation between oropharyngeal infection and the development of DNM. However, the treatment strategy for DNM remains controversial, especially the role of the transthoracic approach. A proposal for a new clinical classification of DNM and surgical management strategies [including minimally invasive approach by video-assisted thoracic surgery (VATS)], based on the progression of mediastinal infection on computed tomography (CT) have been recently proposed by Guan et al. (5) and Yano et al. (6).
The main factors related to mortality are delayed diagnosis, inappropriate or delayed antibiotic therapy, and incorrect cervical and pleuro-mediastinal surgical drainage (7-10). Multidisciplinary approach and coordination among departments have been associated to a reduced risk of mortality (10).
The aim of this retrospective case series study is to describe our experience in a cohort of seven patients diagnosed with DNM. Five of our patients were diagnosed during the COVID pandemic, as of 11 March 2020. We identify the key points that we consider account for the zero-mortality rate in our series. We present this article in accordance with the AME Case Series reporting checklist (available at https://med.amegroups.com/article/view/10.21037/med-23-32/rc).
Case presentation
We retrospectively reviewed the medical records of a cohort of seven consecutive patients treated at Hospital de la Santa Creu i Sant Pau for DNM between March 2019 and July 2022. Due to the limited number of cases included in the study, no statistical analysis was performed. Description and critical data analysis are presented.
Data from medical charts included demographics (age, sex), comorbidities and risk factors (cigarette smoking), origin of infection (odontogenic, tonsils, parapharyngeal), results of the microbiological cultures, days to cervical and mediastinal drainage from the onset of symptoms, inpatient antibiotic treatment, intensive care unit (ICU) length of stay, hospitalization length of stay, type of surgery, need for reoperation, number of patients who underwent tracheostomy, and outcome.
Diagnosis of DNM was performed on the basis of criteria defined by Estrera et al. (2). Clinical evidence of severe oropharyngeal infection; radiographic characteristics of mediastinitis; surgical or post-mortem evidence of DNM, and relationship of the oropharyngeal infection with the development of the DNM.
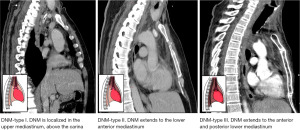
The extent of dissemination of DNM into the mediastinum was based on CT scan findings (Figure 1). Mediastinitis was classified according to Endo’s criteria (11) in type I (focal) mediastinitis (infection limited to the superior mediastinal space, above tracheal bifurcation) and type II (diffuse) mediastinitis that was in turn subdivided into subtype IIA (infection still limited to the anterior inferior mediastinal space) and subtype IIB (infection spread has reached posterior inferior mediastinum) (Figure 2).
A postoperative analytical follow-up was carried out using the C-reactive protein (CRP) as an indicator of poor clinical evolution and to help diagnose postoperative infection and monitor the efficacy of antibiotic therapy. Procalcitonin (PCT) may also be helpful to distinguish between infectious and noninfectious causes of systemic inflammation (12).
Outpatient follow-up within 7 and 30 days of discharge were determined. No patient was readmitted within 30 days of a hospital discharge. There were no losses to follow up.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Drug Research Ethics Committee R-OBS (Code IIBSP-MED-2022-08, Registration No. 22/024) and informed consent was taken from all the patients. The written consents are available for review by the editorial office of this journal.
There were six men and one woman. Ages ranged from 22 to 65 years (mean: 50 years). All the patients rated a predefined set of data groups regarding their inclusion in the study and complete at least 30 days follow-up after discharge.
All patients fulfilled the diagnostic criteria defined by Estrera and colleagues (2). The primary oropharyngeal infection was a peritonsillar abscess in three cases and an odontogenic abscess in four. All patients presented with dysphagia, fever, and respiratory insufficiency associated with a severe cervical infection. Four patients had subcutaneous emphysema. All these symptoms suggested mediastinitis. The delay between onset of primary infection and hospitalization varied from 4 to 12 days (mean: 7 days).
Three patients had associated comorbidities (heart disease, a history of heavy smoking, and high alcohol consumption). One of the three also had diabetes and chronic obstructive pulmonary disease. Four patients had no obvious risk factors.
The delay between the onset of the primary infection and surgery ranged from 5 to 12 days (mean: 7 days). None of the five cases diagnosed during the COVID 19 pandemic were positive for SARS-CoV-2 infection.
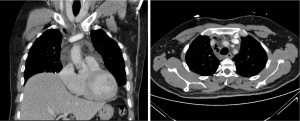
Given the suspected diagnosis, broad-spectrum antibiotic therapy was started, and urgent surgery was indicated. The surgical team included specialists from the otolaryngology, maxillofacial, and thoracic surgery departments. A collar cervicotomy was performed for cervical drainage in all cases. This entailed opening all the involved cervical spaces and draining and debriding the necrotic tissue to control the cervical focus. The surgical approach to draining the mediastinum depends on the extension of the abscess. In all cases, a minimally invasive video-assisted thoracoscopic approach was chosen (transcervical, transthoracic or subxiphoid VATS) (Figure 3). To perform a transthoracic VATS procedure, three or four 5 mm intercostal trocars were required. When it was deemed necessary (mainly to drain large retrosternal collections), subxiphoid and two intercostal approaches were combined (Figure 4) (13). Regarding instrumentation, a 5-mm, 30-degree thoracoscope was used to explore the anterior and the middle mediastinum and the pleural cavity. One or two forceps and a 5 mm advanced bipolar energy system helps to dissect and coagulate the tissue. CO2 insufflation facilitates dissection of the anterior mediastinum, but it should not be higher than 10 mmHg to avoid vena cava and the right atrium during right-sided procedures.

In all cases we observed a cervical abscess with involvement of the parapharyngeal space, the anterior and posterior cervical compartment, and the anterosuperior mediastinum. According to the Endo’s classification (11), an infection localized to the upper mediastinal space above the carina DNM was diagnosed in one case (type I), in five cases the infection extended to the lower anterior mediastinum (type IIA) and in another case it extended to both the anterior and posterior lower mediastinum (type IIB) (Figure 2). In three patients the infection spread into the pleural cavities. DNM localized to the upper mediastinal space above the carina was diagnosed in one case (type I). In five cases the infection extended to the lower anterior mediastinum (type IIA) and in another it extended to both the anterior and posterior lower mediastinum (type IIB) (Figure 2).
All patients underwent surgery to debride and drain the neck, pleural and mediastinal collections.
Table 1 shows the origin of the infection, the spaces involved, the microbiological findings, and the treatment in each case. The isolated organisms were Staphylococcus pyogenes A, Staphylococcus capitis, Streptococo anginosus, Streptococcus constellatus, Streptococus viridans, Bacillus, Prevotela melaninogenica, Prevotela baroninae, Eggarthia catenaformis, and Stackia exigua. In all patients, bacteriologic features revealed polymicrobial infection, with mixed aerobic and anaerobic organisms in three patients, anaerobic organism exclusively in two patients and aerobic organisms exclusively in one patient.
Table 1
| Patients (No.) | Age (years) | Origin of the DNM | Mediastinum involvement according Endo’s classification | Surgery after onset symptoms (days)/COVID-19 pandemic | Culture results | Antibiotic | Medical treatment (days) |
|---|---|---|---|---|---|---|---|
| 1 | 64 | Dental | IIA | 4/no | Streptococcus pyogenes A/Staphylococcus epidermidis and capitis AN | Meropenem/ceftriaxone + clindamycin | 16 |
| 2 | 22 | Parapharyngeal abscess | IIA | 12/yes | Streptococcus anginosus A/Bacilus AN | Meropenem + linezolid/ciprofloxacin + clindamycin | 23 |
| 3 | 65 | Parapharyngeal abcess | IIA | 4/yes | Streptococcus viridans A/Fusobacterium AN | Ceftriaxone + metronidazole/amoxicilli clavulanic acid | 33 |
| 4 | 41 | Parapharyngeal abcess | I | 7/yes | Prevotela melaninogenica, Prevotela baroninae AN | Piperacillin tazobactan + amoxicillin clavulanic acid | 31 |
| 5 | 49 | Dental | IIB | 7/yes | Streptococcus constellatus A/Prevotella baroniae AN | Vancomycin + meropenem + clindamycin/meropenem + fluconazole | 62 |
| 6 | 61 | Dental | IIA | 10/yes | Eggerthia catenaformis AN Slackia exigua AN | Meropenem + vancomycin + clindamycin + anidulafungine + aciclovir | 58 |
| 7 | 51 | Dental | IIA | 5/no | Streptococcus constellatus A | Meropenem + vancomycin | 30 |
DNM, descending necrotizing mediastinitis; COVID-19, coronavirus disease-19; A, aerobic; AN, anaerobic.
One patient (14.2%), who was classified as type I according to the Endo’s classification (11), was treated with transcervical mediastino-thoracoscopy drainage only. In six patients (85.8%) we performed a combined transcervical and a minimal invasive transthoracic approach including intercostal and subxiphoid approaches. In five of the six patients who underwent a transcervical and minimal invasive transthoracic approach, the infection had spread to the lower anterior mediastinum (type IIA). In all five, a right VATS approach was undertaken and a bilateral and/or subxiphoid VATS was required in two cases. In the remaining case the infection had spread to the middle mediastinum and the right pleura (type IIB). In this patient, we performed a transcervical videomediastino-thoracoscopy. After the right paratracheal compartment was dissected and drained we were able to identify and incise the right mediastinal pleural. Once opened, a 30º-5 mm thoracoscope was introduced through the video-mediastinoscope. With the 30º video-thoracoscope we were able to explore and drain the right pleural cavity.
Reoperation was required in 3 (43%) cases [patient number 5, 6 and 7 (Figure 5)]. As expected, these were the patients with the greatest number of comorbidities.
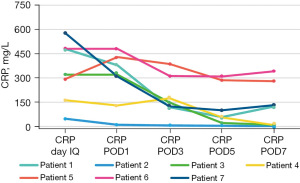
It was indicated for poor control of the general septic syndrome, the presence of pleural empyema and persistent draining cervical and/or mediastinal fluid collections. Two patients underwent two re-interventions, while the third patient underwent four re-interventions. The main parameter that indicated a poor clinical evolution in these patients was an increase in CRP 3 days after appropriate antibiotic treatment was started (Figure 5). In all cases, a new cervical and thoracic CT scan was performed to diagnose and localize drainable abscesses. Cervical and thoracic examinations were carried out simultaneously in all these patients. At the cervical level, the cavities where septated purulent collections had re-formed were debrided; at the thoracic and mediastinal level, minimally invasive surgery re-VATS was performed on demand to locate and debride the purulent collections and placing drains.
Three patients required a tracheostomy. The average length of hospital stay was 22.78±10.05 days (range, 9–40 days). This was divided into 6.4±10.10 days (range, 0–25 days) in the ICU and 16.3±10.1 days in the hospital ward. Three patients had an uneventful postoperative course while four experienced any complication, being the most common of which were dysphagia, internal jugular vein thrombosis, pulmonary embolism, pericarditis, cardiac arrhythmias, and kidney failure.
There were no in-hospital deaths. All patients were discharged safely from hospital.
Discussion
DNM is a severe, potentially fatal form of mediastinitis that can complicate common odontogenic or deep cervical infections. Odontogenic origin is the most commonly reported site of primary infection, usually arising from the second or third molar. Important pathophysiological factors in the extension of deep neck infections to the mediastinum are the effect of gravity, the negative intrathoracic and pleural pressure during inspiration, and the absence of barriers in the fascial planes (14). Diabetes, immunosuppression, and debilitated status are well recognized risk factors (15,16). Introduction of new antibiotics, early diagnosis based on clinical findings and CT images and timely and aggressive multidisciplinary treatment, have substantially contributed to reduce the mortality to less than 10% (10,17-20).
No relationship between COVID-19 infection and an increased incidence of DNM has been reported in the literature. We attribute this fact to the delay of patients in consulting a medical service and, therefore, to the complication of the underlying process.
The etiological organisms are mostly mixed polymicrobial aerobic and anaerobic infections (17). In our series, the organisms isolated in the cultures of drainage fluids were polymicrobial infection in all cases, with mixed aerobic and anaerobic organisms in most patients.
The age of patients in our study ranged from 22 to 65 years (mean: 50 years), with the origin of infection being a parapharyngeal abscess in younger patients and of dental origin in middle-aged patients. In a retrospective review of 43 cases of DNM, Deu-Martín et al. (19) reported that the mean age at presentation was 48 years, similar to the mean age of our patients and the location of the primary infection.
Series in the literature have reported mortality rates due to DNM of up to 40% (1-4,11,14). In our small case series, zero-mortality was achieved. We consider several factors that can be attributed to improving the prognosis of these patients: early diagnosis, multimodality approach together with an aggressive and early surgical intervention, proper airway management, appropriate antibiotic therapy, follow-up with PCT and CRP as inflammatory biomarkers associated with severity of disease, and advanced management in the ICU (19,20).
Early diagnosis: Clinical symptoms are not always clear, and diagnosis is commonly delayed. If mediastinitis is suspected, a CT scan, including the thorax, may help diagnosis and treatment decision-making. In our series, the mean delay between onset of symptoms and hospitalization was 7 days, which is similar to the published in the literature (21,22).
A multimodality approach including a rapid assessment by ENT, thoracic surgeons, and intensivists, and early aggressive surgical intervention are crucial to reduce mortality and morbidity. Surgical approach recommendations are based on the anatomical extent of the infection according to the Endo’s classification. Nevertheless, no definitive surgical treatment procedure has yet been established. While some authors advocate a relatively conservative approach (with and without DNM involving the anterior and/or the posterior mediastinum) with only a limited debridement via cervicotomy plus a transcervical drainage of the infection (including a video-mediastinoscopic approach and insertion of mediastinal and intercostal chest drains) (23-27), others authors clearly support a more aggressive approach consisting of a combination of cervical drainage plus a radical surgical debridement of the mediastinum via thoracotomy or videothoracoscopy if the infection extends to the lower mediastinum (6,9,11,19,22,28-33).
In our series the surgical approach was strictly based on Endo’s classification: one patient with type I-DNM underwent a transcervical mediastino-thoracoscopy drainage only; the other six patients with type IIA-DNM and type IIB-DNM underwent a combined transcervical and a minimal invasive transthoracic (intercostal VATS and/or subxiphoid) approaches. After reviewing our recent experience, we are firmly convinced that the extension of DNM on CT should be the guide for orderly drainage of all the infected spaces. Cervical and paratracheal drainage via a transcervical approach allows the local control of the infection and helps to avoid the spread of infection into the posterior and anterior mediastinum. If the infection spreads into the deep mediastinum, a minimally invasive thoracic approach should be considered as a first option over the open approach. Minimally invasive thoracic surgery techniques allow complex intrathoracic procedures through minimal incisions, thereby decreasing morbidity. This approach allows a more rapid recovery, less surgical trauma and metabolic stress, lower analgesic requirements, shorter hospital stay (34,35).
Frequently, repeated drainage is needed as reported in most published series (2,3,36). In our series reoperations were required in 3 (33.3%) cases. Two patients underwent two re-interventions, while the third patient underwent four re-interventions. All three cases were each time reoperated by re-VATS. Conversion to thoracotomy was not deemed necessary in any case. We consider that minimally invasive surgery at both the cervical and thoracic level definitively contributed to the good results in our series.
Appropriate post-operative care in the ICU is important to manage further complications that may arise due to a prolonged ICU stay. Together with clinical parameters, CRP levels are helpful for monitoring evolution of the infection after the surgical procedure. When there is a good response to treatment, CRP levels decrease within 1–3 days after surgery. Failure to show a decrease in CRP levels in this timeframe is suggestive of treatment failure. As PCT may also be helpful to monitor the clinical evolution and response to antibiotics, it could be evaluated as a potential biomarker. We have not included PCT levels in our series of patients because they were not requested and followed in all of them. However, we do advise the importance of always requesting them given their great predictive value both in the diagnosis and in the follow-up and prognosis of patients with DNM.
In case of a suspected complication or persistent infection, a CT scan will be necessary to confirm and re-evaluate medical or surgical treatment.
Regardless of the number of surgical re-interventions, the complications that our patients presented were not secondary to the type of surgery but to the infection itself. Three patients required tracheostomy due to prolonged intubation, three had dysphagia because of muscular motor discoordination, one developed pericarditis that resolved medically, and one developed myopathy that took 3 months to resolve.
The findings of this study have to be seen in light of some limitations. First, the retrospective nature of the data which could lead to differences in the accuracy or completeness of the results retrieved. Second, the insufficient sample size for statistical measurements and to support widespread changes in clinical practice. Third, the potentially limited external validity of the results because of the study was carried out in a single center.
Conclusions
The key points to reduce the high mortality associated with MND are a rapid multidisciplinary medical and surgical approach. In addition to transcervical drainage, a minimally invasive transthoracic CT-guided approach for surgical treatment of MND is feasible, effective, and less invasive, and should be considered the first option in these patients. Surgical re-interventions in these patients are frequent due to poor infection control, in these cases re-VATS may be a valid option.
Acknowledgments
Part of this work was presented as a poster communication at the annual meeting of the National Congress of the Spanish Society of Pneumology and Thoracic Surgery (SEPAR).
Funding: None.
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://med.amegroups.com/article/view/10.21037/med-23-32/rc
Peer Review File: Available at https://med.amegroups.com/article/view/10.21037/med-23-32/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-23-32/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Drug Research Ethics Committee R-OBS (Code IIBSP-MED-2022-08, Registration No. 22/024) and informed consent was taken from all the patients. The written consents are available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ridder GJ, Maier W, Kinzer S, et al. Descending necrotizing mediastinitis: contemporary trends in etiology, diagnosis, management, and outcome. Ann Surg 2010;251:528-34. [Crossref] [PubMed]
- Estrera AS, Landay MJ, Grisham JM, et al. Descending necrotizing mediastinitis. Surg Gynecol Obstet 1983;157:545-52. [PubMed]
- Freeman RK, Vallieres E, Verrier ED, et al. Descending necrotizing mediastinitis: an analysis of the effects of serial debridement on patient mortality. J Thorac Cardiovasc Surg 2000;119:260-7. [Crossref] [PubMed]
- Pearse HE. Mediastinitis following cervical suppuration. Ann Surg 1938;108:588-611. [Crossref] [PubMed]
- Guan X, Liang X, Liang X, et al. A new classification of descending necrotizing mediastinitis and surgical strategies. Ann Transl Med 2021;9:356. [Crossref] [PubMed]
- Yano M, Numanami H, Akiyama T, et al. Distribution of descending necrotizing mediastinitis and efficacy of distribution-specific drainage. J Thorac Dis 2020;12:2380-7. [Crossref] [PubMed]
- Sumi Y. Descending necrotizing mediastinitis: 5 years of published data in Japan. Acute Med Surg 2015;2:1-12. [Crossref] [PubMed]
- De Palma A, Cantatore MG, Di Gennaro F, et al. Multidisciplinary Approach in the Treatment of Descending Necrotizing Mediastinitis: Twenty-Year Single-Center Experience. Antibiotics (Basel) 2022;11:664. [Crossref] [PubMed]
- Marty-Ané CH, Berthet JP, Alric P, et al. Management of descending necrotizing mediastinitis: an aggressive treatment for an aggressive disease. Ann Thorac Surg 1999;68:212-7. [Crossref] [PubMed]
- Ho CY, Chin SC, Chen SL. Management of Descending Necrotizing Mediastinitis, a Severe Complication of Deep Neck Infection, Based on Multidisciplinary Approaches and Departmental Co-Ordination. Ear Nose Throat J 2022; Epub ahead of print. [Crossref] [PubMed]
- Endo S, Murayama F, Hasegawa T, et al. Guideline of surgical management based on diffusion of descending necrotizing mediastinitis. Jpn J Thorac Cardiovasc Surg 1999;47:14-9. [Crossref] [PubMed]
- Binnie A, Lage J, Dos Santos CC. How can biomarkers be used to differentiate between infection and non-infectious causes of inflammation? Evidence-Based Practice of Critical Care 2020:319-24.
- Kumar A, Parshad R, Suhani S, et al. Descending Necrotizing Mediastinitis: A Surgical Challenge Managed Using Subxiphoid VATS. ACS Case Reviews in Surgery 2022;3:6-10.
- Kang SK, Lee S, Oh HK, et al. Clinical features of deep neck infections and predisposing factors for mediastinal extension. Korean J Thorac Cardiovasc Surg 2012;45:171-6. [Crossref] [PubMed]
- Sancho LM, Minamoto H, Fernandez A, et al. Descending necrotizing mediastinitis: a retrospective surgical experience. Eur J Cardiothorac Surg 1999;16:200-5. [Crossref] [PubMed]
- Mathieu D, Neviere R, Teillon C, et al. Cervical necrotizing fasciitis: clinical manifestations and management. Clin Infect Dis 1995;21:51-6. [Crossref] [PubMed]
- Weaver E, Nguyen X, Brooks MA. Descending necrotising mediastinitis: two case reports and review of the literature. Eur Respir Rev 2010;19:141-9. [Crossref] [PubMed]
- Roccia F, Pecorari GC, Oliaro A, et al. Ten years of descending necrotizing mediastinitis: management of 23 cases. J Oral Maxillofac Surg 2007;65:1716-24. [Crossref] [PubMed]
- Deu-Martín M, Saez-Barba M, López Sanz I, et al. Mortality risk factors in descending necrotizing mediastinitis. Arch Bronconeumol 2010;46:182-7. [PubMed]
- Wakahara T, Tanaka Y, Maniwa Y, et al. Successful management of descending necrotizing mediastinitis. Asian Cardiovasc Thorac Ann 2011;19:228-31. [Crossref] [PubMed]
- Ma C, Zhou L, Zhao JZ, et al. Multidisciplinary treatment of deep neck infection associated with descending necrotizing mediastinitis: a single-centre experience. J Int Med Res 2019;47:6027-40. [Crossref] [PubMed]
- Putra AM, Romolo H, Bunga Syafina A, et al. Descending necrotizing mediastinitis: Management and controversies. Cardiovascular and Thoracic Open 2016;2:1-5. [Crossref]
- Nakamori Y, Fujimi S, Ogura H, et al. Conventional open surgery versus percutaneous catheter drainage in the treatment of cervical necrotizing fasciitis and descending necrotizing mediastinitis. AJR Am J Roentgenol 2004;182:1443-9. [Crossref] [PubMed]
- Sumi Y, Ogura H, Nakamori Y, et al. Nonoperative catheter management for cervical necrotizing fasciitis with and without descending necrotizing mediastinitis. Arch Otolaryngol Head Neck Surg 2008;134:750-6. [Crossref] [PubMed]
- Hsu RF, Wu PY, Ho CK. Transcervical drainage for descending necrotizing mediastinitis may be sufficient. Otolaryngol Head Neck Surg 2011;145:742-7. [Crossref] [PubMed]
- Jayasekera BA, Dale OT, Corbridge RC. Descending necrotising mediastinitis: a case report illustrating a trend in conservative management. Case Rep Otolaryngol 2012;2012:504219. [Crossref] [PubMed]
- Fukuchi M, Suzuki O, Nasu D, et al. Descending Necrotizing Mediastinitis Treated with Tooth Extractions following Mediastinal and Cervical Drainage. Case Rep Gastroenterol 2015;9:311-6. [Crossref] [PubMed]
- Iwata T, Sekine Y, Shibuya K, et al. Early open thoracotomy and mediastinopleural irrigation for severe descending necrotizing mediastinitis. Eur J Cardiothorac Surg 2005;28:384-8. [Crossref] [PubMed]
- Singhal P, Kejriwal N, Lin Z, et al. Optimal surgical management of descending necrotising mediastinitis: our experience and review of literature. Heart Lung Circ 2008;17:124-8. [Crossref] [PubMed]
- Yun JS, Lee CH, Na KJ, et al. Surgical Experience with Descending Necrotizing Mediastinitis: A Retrospective Analysis at a Single Center. J Chest Surg 2023;56:35-41. [Crossref] [PubMed]
- Son HS, Cho JH, Park SM, et al. Management of descending necrotizing mediastinitis using minimally invasive video-assisted thoracoscopic surgery. Surg Laparosc Endosc Percutan Tech 2006;16:379-82. [Crossref] [PubMed]
- Kocher GJ, Hoksch B, Caversaccio M, et al. Diffuse descending necrotizing mediastinitis: surgical therapy and outcome in a single-centre series. Eur J Cardiothorac Surg 2012;42:e66-72. [Crossref] [PubMed]
- Makeieff M, Gresillon N, Berthet JP, et al. Management of descending necrotizing mediastinitis. Laryngoscope 2004;114:772-5. [Crossref] [PubMed]
- Min HK, Choi YS, Shim YM, et al. Descending necrotizing mediastinitis: a minimally invasive approach using video-assisted thoracoscopic surgery. Ann Thorac Surg 2004;77:306-10. [Crossref] [PubMed]
- Cho JS, Kim YD. Treatment of mediastinitis using video-assisted thoracoscopic surgery. Eur J Cardiothorac Surg 2008;34:520-4. [Crossref] [PubMed]
- Taylor M, Patel H, Khwaja S, et al. Descending cervical mediastinitis: the multidisciplinary surgical approach. Eur Arch Otorhinolaryngol 2019;276:2075-9. [Crossref] [PubMed]
Cite this article as: Venegas Pizarro MDP, Martínez Téllez E, León Vintró X, Quer Agustí M, Trujillo-Reyes JC, Libreros-Niño A, Planas Cánovas G, Belda-Sanchis J. Descending necrotizing mediastinitis: key points to reduce the high associated mortality in a consecutive case series. Mediastinum 2024;8:8.